by

Engineers in the Center for Precision Engineering for Health (CPE4H) are focusing on innovations in diagnostics and delivery, cellular and tissue engineering, and the development of new devices that integrate novel materials with human tissues. Below is an excerpt from “Going Small to Win Big: Engineering Personalized Medicine,” featuring the research from the laboratory of Jenny Jiang, J. Peter and Geri Skirkanich Associate Professor of Innovation in Bioengineering.
The Challenge
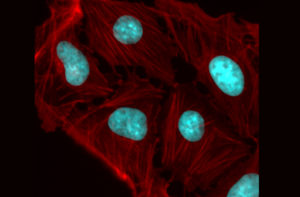
In order to create personalized immune therapies, researchers need to untangle what is happening between an individual patient’s immune cells and the antigens that they interact with on a molecular level. Immune cell-antigen interactions need to be understood in four different areas in order to create a full picture: the unique genetic sequence of the T cell’s antigen receptors, the antigen specificity of that cell, and both the gene and protein expression of the same cell.
The Status Quo
Prior methods of understanding interactions between T cells and antigens could only get a picture of one or two of these four elements because of technology constraints. Other roadblocks included that cells cultured or engineered in a laboratory setting are not in a natural environment so they won’t express genes or proteins in the way T cells would in the body, and technologies that assess the antigen specificity of T cells were not cost-effective for looking at large numbers of antigens.
The Jiang Lab’s Fix
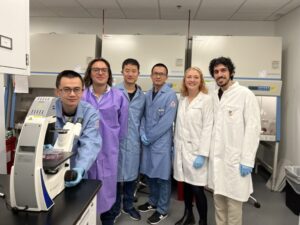
The lab of Jenny Jiang, J. Peter and Geri Skirkanich Associate Professor of Innovation in Bioengineering, developed a technology called TetTCR-SeqHD, which solves these problems. Using this technology, scientists can now simultaneously profile samples of large numbers of single T cells in the four dimensions using high- throughput screening.
The Jiang Lab’s technology is essentially a method for getting a “full-body scan” of an individual’s T cells and creates a catalog of the different types of T cells and the antigens they respond (or don’t respond) to, paving the way for the ability to better target immune therapies to an individual patient.
“Individual T cells are unique, and that’s the challenge of using one treatment to fit all,” says Jiang. “Identifying antigen specificity and creating therapies that target that specificity in an individual’s T cells will be key to truly personalizing immune therapies in the future.”