Using Stem Cells to Repair Damaged Tissue
Repairing heart tissue after a heart attack is a major focus of tissue engineering. A key challenge here is keeping grafted cardiomyocytes in place within the tissue to promote repair. As we reported a couple of weeks ago, using tissue spheroids and nanowires is one approach to overcome this challenge. Another approach involves manipulating the cell cycle — the process by which normal cells reproduce, grow, and eventually die.
Making Music
People and Places
Oncology/Engineering Review Published

Michael Mitchell, Ph.D., who will arrive in the Spring 2018 semester as assistant professor in the Department of Bioengineering, is the first author on a new review published in Nature Reviews Cancer on the topic of engineering and the physical sciences and their contributions to oncology. The review was authored with Rakesh K. Jain, Ph.D., who is Andrew Werk Cook Professor of Radiation Oncology (Tumor Biology) at Harvard Medical School, and Robert Langer, Sc.D., who is Institute Professor in Chemical Engineering at the David H. Koch Institute for Integrative Cancer Research at MIT. Dr. Mitchell is currently in his final semester as a postdoctoral fellow at the Koch Institute and is a member of Dr. Langer’s lab at MIT.
The review focuses on four key areas of development for oncology in recent years: the physical microenvironment of the tumor; technological advances in drug delivery; cellular and molecular imaging; and microfluidics and microfabrication. Asked about the review, Dr. Mitchell said, “We’ve seen exponential growth at the interface of engineering and physical sciences over the last decade, specifically through these advances. These novel tools and technologies have not only advanced our fundamental understanding of the basic biology of cancer but also have accelerated the discovery and translation of new cancer therapeutics.”
Week in BioE (October 20, 2017)

Fetal Repair Without Surgery?
Spina bifida is a fairly common type of birth defect caused by incomplete closure of the backbone and tissue surrounding the spinal cord. Fetal surgery can repair the defect before delivery, but this invasive surgery can lead to high risk preterm delivery.
A new material may dramatically reduce the invasiveness of surgery needed to correct spina bifida. In a new article in Macromolecular Bioscience, surgeons and bioengineers from the University of Colorado report on one of these alternatives. One of the lead authors was Daewon Park, Ph.D., assistant professor of bioengineering. Dr. Park and his colleagues developed a reverse thermal gel, which is an injectable liquid that forms a gel at higher temperatures when injected into the body. Ultimately a gel like this one could be injected at or near the spine, where it would cover the defect in a spina bifida patient, harden into a gel, and ultimately repair the defect by deploying stem cells or engineered tissue.
The research team’s most recent study indicates that their gel retained its stability in amniotic fluid and was compatible with neural tube cells. They also tested the gel in two animal models, with successful results. The gel is still far from being used in actual fetal surgery cases, but the authors will continue to test the gel under conditions increasingly similar to the human amniotic sac.
Building Better Brains
UCLA scientists have developed an improved system for generating brain structures from stem cells. The team of scientists, led by Bennett G. Novitch, Ph.D., professor of neurobiology at UCLA, report their findings in Cell Reports. Importantly, the methods used by Dr. Novitch and his colleagues fine-tuned and simplified earlier efforts in this area, developing a method that did not require any specific reactors to generate the tissue. They were also able to generate tissue resembling the basal ganglia for the first time, indicating promise for using these tissues to model diseases affecting that part of the brain, including Parkinson’s disease.
Next, the authors demonstrated the usefulness of these “organoids” in modeling damage due to Zika virus. After exposing the generated organoids to Zika, the authors measured the cellular responses of the tissue, demonstrating the ability to use these tissues to model the disease. Given the recent epidemic of Zika virus in the Western Hemisphere, which focused attention on the virus’s effects on the human brain, in addition to microcephaly and other birth defects when the disease is transmitted from pregnant mothers to their children, understanding how Zika affects the developing brain is key to determining how to prevent the damage it causes and possibly repairing it. Reliable models of brain development are necessary, and the UCLA team’s findings seem to indicate that they’ve found one.
Rebuilding Brain Circuits After Injury
Seeing Inside the Body
Implants That Grow With Chilren
Say What?
Lagrange Goes to Dani Bassett

Danielle S. Bassett, Eduardo D. Glandt Faculty Fellow and Associate Professor in the University of Pennsylvania’s Department of Bioengineering, is the recipient of the 2017 Lagrange-CRT Foundation Prize. The prize, given by the Institute for Scientific Interchange Foundation in Turin, Italy, was created to encourage and honor researchers working in the field of complex systems.
Complex systems feature many interconnected parts whose individual behavior influences the outcomes of the whole. Examples include social media networks, ecological webs, stock markets, and in Bassett’s case, the brain. Her research maps and analyzes the networks of neurons that enable all manners of cognitive abilities, as well as how those networks evolve during development or malfunction in disease.
The prize comes with an award of €50,000, or roughly $60,000. It will be formally presented to Bassett at a ceremony in Turin next week. Bassett is the first woman to be the sole recipient of the prize since its inception in 2008. Lada Adamic won it alongside Xavier Gabaix in 2012.
Read more at the SEAS blog on Medium.
Chairs for BMES ’19 to Include Burdick
 Jason Burdick, Ph.D., who is a professor in the University of Pennsylvania’s Department of Bioengineering, has been named one of the three chairs of the 2019 annual meeting of the Biomedical Engineering Society (BMES), which be held here in Philadelphia on October 16-19. Dr. Burdick will share this position with two other Philadelphians: Alisa Morss Clyne, Ph.D., an associate professor of mechanical engineering and mechanics at Drexel University; and Ruth Ochia, Ph.D., an associate professor of instruction in bioengineering at Temple University. Drs. Burdick, Clyne, and Ochia will share the responsibility for planning the meeting and chairing it once it is in session.
Jason Burdick, Ph.D., who is a professor in the University of Pennsylvania’s Department of Bioengineering, has been named one of the three chairs of the 2019 annual meeting of the Biomedical Engineering Society (BMES), which be held here in Philadelphia on October 16-19. Dr. Burdick will share this position with two other Philadelphians: Alisa Morss Clyne, Ph.D., an associate professor of mechanical engineering and mechanics at Drexel University; and Ruth Ochia, Ph.D., an associate professor of instruction in bioengineering at Temple University. Drs. Burdick, Clyne, and Ochia will share the responsibility for planning the meeting and chairing it once it is in session.
“I am very happy to be appointed as a program chair for the 2019 BMES meeting in Philadelphia, along with Alisa Morss Clyne of Drexel University and Ruth Ochia of Temple University,” Dr. Burdick said when asked about the honor. “The three of us felt that it was important to represent the various biomedical engineering research and education programs within the city of Philadelphia, since the meeting will be held here. There is such a wealth of biomedical engineering efforts in Philly that provides great opportunities to engage in outreach and interaction with both the community and local industry during the meeting.”
Week in BioE (October 13, 2017)
Seeing and Repairing Damaged Heart Vessels
Two common diagnostic procedures in cardiology are intravascular ultrasound and cardiac angiography. These procedures are performed to quantify the amount of plaque affecting a patient’s blood vessels. This information is vital because it helps to determine how advanced heart degree is, as well as guiding treatment planning and even the course of bypass surgery. However, the current technologies used for these procedures have significant limitations. Although conventional angiography can help to quantify the plaque burden, it does not offer any information about how much of the diameter of a vessel is blocked. Intravascular ultrasound is very good at quantifying plaque burden, but it is poor at identifying smaller features of compromised blood vessels.
One solution suggested to these issues is the combination of these imaging technologies into a single multimodal technique. Scientists led by Laura Marcu, Ph.D., professor of biomedical engineering at the University of California, Davis, invented a method combining intravascular ultrasound with multispectral fluorescence lifetime imaging (FLIM). As published in Scientific Reports, the device resembles a typical cardiac catheter but contains an optical fiber within the catheter that emits fluorescent light to characterize the plaque components before treatment.
Dr. Marcu and her colleagues tested their new device in live pigs and in human coronary arteries obtained from cadavers. The fluorescence data acquired with the device were comparable to those acquired with traditional fluorescence angiography. Moreover, the device could acquire data without having to administer a contrast agent, which can be dangerous in some patients due to allergies or weakened kidneys. The authors are currently seeking FDA approval to test their combined catheter in humans.
In addition to treating vessels before a heart attack can occur, there is new work showing how to efficiently repair heart tissue after a heart attack. A team of scientists collaborating among Clemson University, the Medical University of South Carolina, the University of South Carolina, and the University of Chicago has received a $1.5 million grant from the National Institutes of Health to examine a treatment that combines stem cells with nanowires. The principal investigator on the grant is Ying Mei, Ph.D., who is assistant professor of bioengineering at Clemson. Dr. Mei’s team mixes stem cells with nanowires so that they form spheroids that are larger than single cells and thus less likely to wash away. In addition, the investigators hope that the spheroids will mitigate the issue of the transplanted cells and the recipient’s heart beating at different rhythms. If successful, the group’s treatment paradigm could be a major step forward in stem cell therapies and cardiology.
Look, Up in the Sky!
Drones became famous when deployed on battlefields for the first time a decade ago. Since then, they’ve been adopted as a technology for a variety of purposes. For example, Amazon introduced delivery drones almost a year ago, and it has plans to expand its drone fleet enormously in coming years. It was only a matter of time before engineers began to imagine medical applications for drones.
Engineers in Australia and Iraq recently investigated whether a drone could be used to monitor cardiorespiratory signals remotely. They reported their findings in BioMedical Engineering OnLine. The authors used imaging photoplethysmography (PPG), which employs a video camera to detect visual indications on the skin of heart activity. They also applied advanced digital processing technology due to the tendency of PPG to be affected by sound and movement in the area of detection. By testing the combined technologies in 15 healthy volunteers, the authors found that their data compared well with several traditional techniques for monitoring vital signs. Among the possible applications that the authors imagine for this technology is battlefield triage performed remotely using drones. In the meantime, they will seek to fine-tune the technology’s abilities.
Concussion Distressingly Common
A research letter published in a recent issue of JAMA reports that a study conducted in Canada found that one in five adolescents sustained a concussion on at least one occasion. Of the approximately 20% of the study respondents who had experienced concussions, one quarter had suffered more than one. The letter is particularly relevant to the United States because of the similar popularity in Canada of contact and semicontact sports such as ice hockey and football. In addition, the study included more than 13,000 teenagers, lending significantly reliability to the conclusions.
Ending the Time of Cholera
Although largely eradicated in the developed world, cholera remains a major public health issue in the Global South and other parts of the developing world. The disease is a bacterial infection that causes severe gastrointestinal distress. Because the disease is transmitted via water, effective public sanitation is a core requirement of an effective prevention campaign.
One technology being deployed in this fight is a smartphone microfluidics platform that can determine the presence of the pathogen that causes cholera in a sample and report the data almost immediately to public health authorities. This technology was produced by a company called PathVis, which was spun off at Purdue University based on science produced the laboratories of Tamara Kinzer-Ursem, Ph.D., and Jacqueline Linnes, Ph.D., both of whom are assistant professors in Purdue’s Weldon School of Biomedical Engineering. There are plans to test PathVis in Haiti and to expand it to detect other diseases in the future.
The Latest on CRISPR
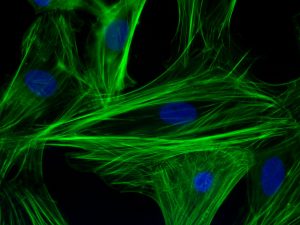
CRISPR/Cas9 is the biggest bioengineering story to come along in some time — certainly the biggest in genetic engineering. But the mere fact that it’s here and already being used in animals and in human cell lines doesn’t mean that the story is over. For instance, the Cas9 protein, which CRISPR deploys as part of its gene editing process, is currently developed most often using a viral vector. However, this system of delivery has certain drawbacks, not the least of which is a host immune system response when levels of the deployed viral vector reach the levels necessary for CRISPR to work.
A recent study published in Nature Biomedical Engineering reports on the successful use of gold nanoparticles to deliver Cas9. The new delivery system, called CRISPR-Gold, could obviate the need to use a viral vector as part of the CRISPR induction process. So far, the authors, led by University of California, Berkeley, bioengineers Irina Conboy, Ph.D., and Niren Murthy, Ph.D., have only used CRISPR-Gold in mice, but their successful results indicate that nonviral delivery with CRISPR is possible, so CRISPR could be used for more than previously thought.
Week in BioE (October 6, 2017)
We Bleed Green
 Biomechanics is a subdiscipline within bioengineering with many applications that include studying how tissue forms and grows during development (see our profile of incoming faculty member Alex Hughes to learn more) and determining how the ‘imprint’ of spine-based pain can be treated with anti-inflammatory medication (see story here on work from the lab of Dr. Beth Winkelstein). Understanding and analyzing human performance are other areas of biomechanics application. On September 24, Eagles kicker Jake Elliott set a team record when he kicked a 61 yard field goal at the end of regulation time to beat the Giants. Marking the achievement, the Philadelphia Inquirer featured an interview with Dr. Chase Pfeifer, a biomedical engineer from the University of Nebraska-Lincoln (UNL), to find out what factors contribute to a successful field goal from this distance. Pfeifer has both knowledge and experience with this question; he was a backup kicker for the Florida State Seminoles as an undergraduate. In the Inquirer, Dr. Pfeifer explained to readers the biophysics behind Elliott’s record kick.
Biomechanics is a subdiscipline within bioengineering with many applications that include studying how tissue forms and grows during development (see our profile of incoming faculty member Alex Hughes to learn more) and determining how the ‘imprint’ of spine-based pain can be treated with anti-inflammatory medication (see story here on work from the lab of Dr. Beth Winkelstein). Understanding and analyzing human performance are other areas of biomechanics application. On September 24, Eagles kicker Jake Elliott set a team record when he kicked a 61 yard field goal at the end of regulation time to beat the Giants. Marking the achievement, the Philadelphia Inquirer featured an interview with Dr. Chase Pfeifer, a biomedical engineer from the University of Nebraska-Lincoln (UNL), to find out what factors contribute to a successful field goal from this distance. Pfeifer has both knowledge and experience with this question; he was a backup kicker for the Florida State Seminoles as an undergraduate. In the Inquirer, Dr. Pfeifer explained to readers the biophysics behind Elliott’s record kick.
Dr. Pfeifer assures readers that there’s more to kicking a 61-yard field goal than strong muscles. He explains, “The timing of muscle activation was actually more important than muscle strength in achieving that higher foot velocity.” Four muscle groups were activated by Elliott to set his record. In addition, Pfeifer’s colleague at UNL, Professor Tim Gay of the physics department, explained to the Inquirer how the climatic conditions favored Elliott’s success. Specifically, since it was a hot day, the air was less dense, allowing for longer kick distances.
Speaking of football, a new article in Annals of Biomedical Engineering offers some hope for NFL players and the league itself in the wake of growing awareness and concern about chronic traumatic encephalopathy (CTE). The increased focus on CTE has resulted in increased research on the condition and its prevention. Real-time measurement of impact energy in head injuries has, until now, relied on measurements of the motion of the head or helmet, rather than measuring the impact energy directly.
In the Annals article, scientists from Brigham Young University, including David T. Fullwood, Ph.D., professor of mechanical engineering, report on the testing of a new sensor used to measure the impact event. The authors implanted nano-composite foam (NCF) sensors into football helmets and then submitted the helmets to two dozen drop tests. The data collected from the foam sensors were compared to two of the most widely used indices to measure head injury risk, achieving excellent correlation (>90%) with injury risk indicators. The authors intend to test newer models of the sensors in the future, as well as in vivo testing.
Breast Cancer News
Despite significant advances in diagnosis and treatment, breast cancer remains the most common cancer in women. More than 300,000 women are newly diagnosed in the United States each year. Maximizing the effectiveness of treatment involves early detection of the tumor and its metastasis. Imaging plays a key role in this process. However, early tumors are very small, making their detection quite difficult.
In response to this challenge, Zheng-Rong Lu, Ph.D., the M. Frank Rudy and Margaret Domiter Rudy Professor of Biomedical Engineering at Case Western Reserve University, has coauthored a paper recently published in Nature Communications showing that a newly developed type of molecule could be used for highly sensitive magnetic resonance imaging (MRI) to detect and stratify early breast tumors.
Dr. Lu and his colleagues engineered molecules called fullerenes, which are hollow, spherical molecules of carbon. The team embedded gadolinium, a rare earth metal that is easily detected with MR imaging, into the fullerene to create metallofullerenes. They tested these metallofullerenes both in vitro and in a mouse model to determine how well they enhanced the ability of MRI to detect tumors. Metallofullerene particles could not only distinguish cancers more effectively on MRI, but they could also distinguish more aggressive tumor types from less aggressive ones. In addition, they found that metallofullerenes rapidly cleared from the body via the kidneys, ensuring that these agents would pose minimal toxicity risk. If this technology proves effective in humans, it could significantly improve the early detection of breast cancer and, in turn, survival rates.
One possible risk for breast cancer patients is the metastasis of the cancer to other body regions. Scientists at Cornell identified a mineral process underlying breast cancer metastasis to bones, reporting their findings in PNAS. Led by Claudia Fischbach-Teschl, Ph.D., associate professor of biomedical engineering at Cornell, the authors investigated how hydroxylapatite — a naturally occurring mineral — participates in metastasis.
Dr. Fischbach-Teschl and her colleagues used X-ray scattering and Raman spectroscopy to examine the nanostructures of hydroxylapatite in the bones of mice with and without breast cancer. They found that bones were more likely to be metastasized by primary breast tumors if the hydroxylapatite crystals in them were less mature. Before the cancer spreads to the bone, the authors found that the cancer “communicates” with these immature crystals, preparing sites in the bone to which the cancer can spread.
With 80% of metastatic breast cancer cases spreading to the bones, the discovery of the Cornell team could contribute enormously to preventing metastasis — not only of breast cancer but also of any cancer with a greater likelihood of spreading to the bones.
A Review of Glucose Monitoring Technology
Our ability to treat diabetes has consistently improved over the years, but the need for patients with the disease to monitor their blood glucose requires either multiple needle pricks or invasive insulin pumps. However, several technologies are in development around the world to make blood glucose monitoring less cumbersome. In a new article published in Bioengineering, engineers in the United Arab Emirates offer a review of the latest technologies, including analytic methods that could streamline decisions on doses of insulin to offset high glucose levels.
People and Places
The University of California, Davis, opened its Molecular Prototyping and BioInnovation Laboratory (MPBIL) in 2014. Since then, the “biomaker lab” has stood as an example of the future of biotechnology education. In collaboration with UCD’s First-Year Seminar Program, the MPBIL has launched a student-designed pilot course that has thus far yielded three seminars. You can read more about UCD’s innovative program at their Web site.
To promote diversity in engineering, the cosmetics company L’Oréal started the L’Oréal USA For Women in Science Program, which awards Changing the Face of STEM mentoring grants. Among this year’s recipients is John Hopkins University’s Sridevi Sarma, Ph.D. Dr. Sarma, who is an associate professor of biomedical engineering, will use her grant in collaboration with the Girls Scouts of Central Maryland to promote physics education for young women. Congratulations to her!
