Neurological disorders such as epilepsy, Alzheimers, Parkinson’s and certain forms of dementia are the leading cause of disability and second-leading cause of disease worldwide. These disorders disproportionately affect low-resourced communities due to lack of access to specialized healthcare, and many of these complex diseases lack curative solutions. The need to address neurological disorders is high, yet current diagnostics and treatments are not effective for preventative or personalized care and are not accessible or affordable enough to meet the needs of more than 3 billion people living with neurological disorders.
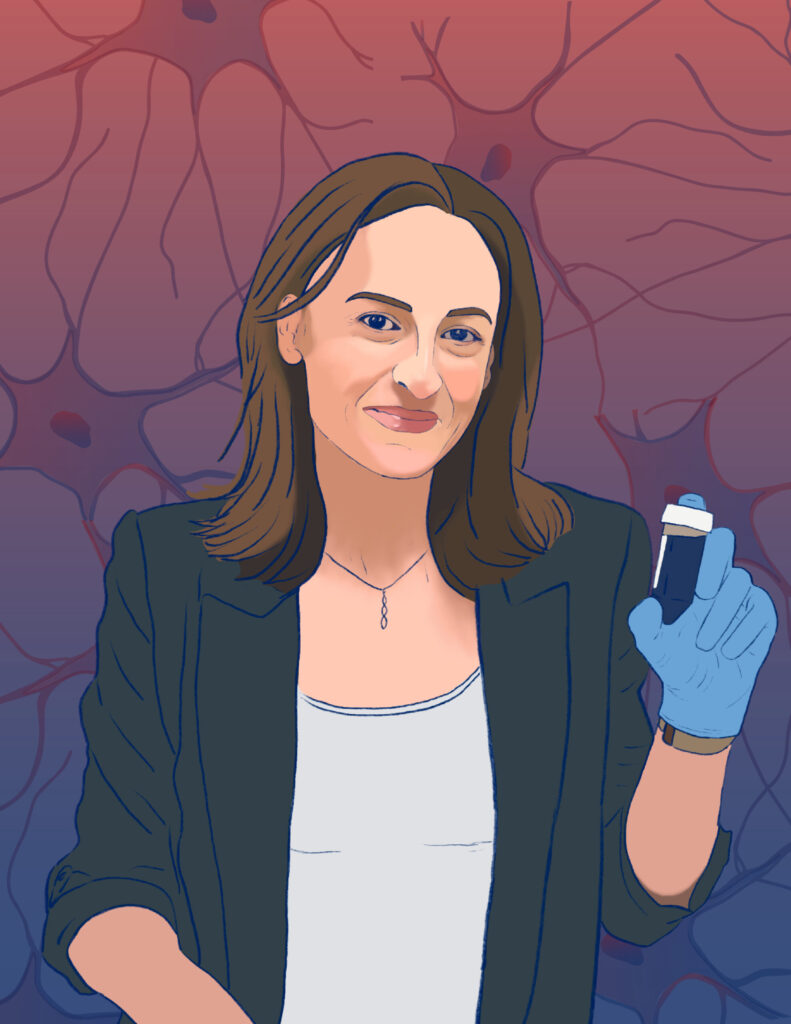
Flavia Vitale, Associate Professor in Bioengineering in Penn Engineering and in Neurology in Penn Medicine, works to meet this need, developing accessible and affordable solutions for the diagnosis, treatment and rehabilitation of people with neurological disorders.
“I started my research career in biomedical engineering hoping to one day help humanity,” says Vitale, who is also a 2024 recipient of a National Science Foundation (NSF) CAREER Award for her work. “But it wasn’t until I gained a more diverse skill set during my doctoral and postdoctoral research across chemical engineering and materials science that I was able to do that in a real way.”
Vitale’s multidisciplinary skills are what allow her to develop devices that help people living with brain disorders. The CAREER Award is now helping her further apply those skills and actualize some of her first long-term research projects at Penn.
“This CAREER Award will support my lab’s current research in leveraging innovation in materials and fabrication approaches to develop devices that are able to interface with and control different chemical and electrical signals inside the brain,” she says.
Focused primarily on understanding the brain activity involved in epilepsy-induced seizures, Vitale aims to design and develop brain-interface devices to pinpoint and suppress uncontrolled brain activity to prevent seizures from happening. Her work will lead to revolutionary health care for the 30% of epilepsy patients whose conditions are drug resistant. Currently those patients either wait out the uncontrolled brain activity and oftentimes life-threatening convulsions, or hope to be eligible for invasive surgeries to remove the part of the brain where seizures originate or to implant the seizure-controlling devices that are currently available.
Read the full story in Penn Engineering Today.









 New research from
New research from