Microscopic Magnets Reduce Pain

Drugs are commonly injected directly into an injury site to speed healing. For chronic pain, clinicians can inject drugs to reduce inflammation in painful joints, or can inject nerve blockers to block the nerve signals that cause pain. In a recent study, a group from UCLA developed a technique to deform a material surrounding nerve fibers to trigger a response in the fibers that would relieve pain. The combination of mechanics and treatment – i.e., ‘mechanoceuticals’ – is a clever way to trick fibers and reverse painful symptoms. Done without any injections and simply controlling magnetic fields outside the body, this approach can be reused as necessary.
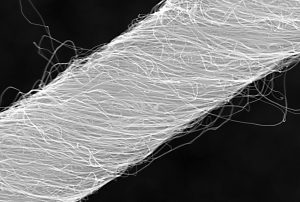
The design of this mechanoceutical was completed by Dino Di Carlo, PhD, Professor of Bioengineering, and his team at UCLA’s Sameuli School of Engineering. By encasing tiny, magnetic nanoparticles within a biocompatible hydrogel, the group used magnetic force to stimulate nerve fibers and cause a corresponding decrease in pain signals. This promising development opens up a new approach to pain management, one which can be created with different biomaterials to suit different conditions, and delivered “on demand” without worrying about injections or, for that matter, any prescription drugs.
Understanding the Adolescent Brain
It’s no surprise that adults and adolescents often struggle to understand one another, but the work of neurologists and other researchers provides a possible physical reason for why that might be. Magnetic resonance elastrography (MRE) is a tool used in biomedical imaging to estimate the mechanical properties, or stiffness, of tissue throughout the body. Unexpectedly, a recent study suggests that brain stiffness correlates with cognitive ability, suggesting MRE may provide insight into patients’ behavior, psychology, and psychiatric state.
A new paper in Developmental Cognitive Neuroscience published the results of a study using MRE to track the relative “stiffness” vs. “softness” of adult and adolescent brains. The University of Delaware team, led by Biomedical Engineering Assistant Professor Curtis Johnson, PhD, and his doctoral student Grace McIlvain, sampled 40 living subjects (aged 12-14) and compared the properties to healthy adult brains.
The study found that children and adolescent brains are softer than those of adults, correlating to the overall malleability of childhood development. The team hopes to continue their studies with younger and older children, looking to demonstrate exactly when and how the change from softness to stiffness takes place, and how these properties correspond to individual qualities such as risk-taking or the onset of puberty. Eventually, establishing a larger database of measurements in the pediatric brain will help further studies into neurological and cognitive disorders in children, helping to understand conditions such as multiple sclerosis, autism, and cerebral palsy.
Can Nanoparticles Replace Stents?
Researchers and clinicians have made amazing advances in heart surgery. Stents, in particular, have become quite sophisticated: they are used to both prop open clogged arteries as well as deliver blood-thinning medication slowly over days to weeks in the area of the stent. However, the risk of blood clotting increases with stents and the blood vessels can constrict over time after the stent is placed in the vessel.
A recent NIH grant will support the design of a stent-free solution to unclog blood vessels. Led by Shaoqin Gong, PhD, Vilas Distinguished Professor of Biomedical Engineering at UW-Madison, the team used nanoparticles (or nanoclusters) to directly target the affected blood vessels and prevent regrowth of the cells post-surgery, eliminating the need for a stent to keep the pathways open. These nanoclusters are injected through an intravenous line, further reducing the risks introduced by the presence of the stent. As heart disease affects millions of people worldwide, this new material has far-reaching consequences. Their study is published in the September edition of Biomaterials.
NIST Grant Supports
The National Institute of Standards and Technology (NIST) awarded a $30 million grant to Johns Hopkins University, Binghamton University, and Morgan State University as part of their Professional Research Experience Program (PREP). Over five years, this award will support the collaboration of academics from all levels (faculty, postdoc, graduate, and undergraduate) across the three universities, enabling them to conduct research and attend NIST conferences.
The principal investigator for Binghamton U. is Professor and Chair of the Biomedical Engineering Department, Kaiming Ye, PhD. Dr. Ye is also the Director of the Center of Biomanufacturing for Regenerative Medicine (CBRM), which will participate in this collaborative new enterprise. Dr. Ye hopes that this grant will create opportunities for academics and researchers to network with each other as well as to more precisely define the standards for the fields of regenerative medicine and biomaterial manufacturing.
People and Places
The A. James Clark Scholars Program has been established in the School of Engineering and Applied Science at the University of Pennsylvania with an extraordinary $15 million gift from the A. James & Alice B. Clark Foundation. It is the largest one-time gift to undergraduate support in the University’s history. The Clark Scholars Program will provide financial aid and create a new academic program for undergraduate engineering students.
The gift honors the late A. James Clark, former CEO of Clark Enterprises and Clark Construction Group LLC, one of the country’s largest privately-held general building contractors. It is designed to prepare future engineering and business leaders, with an emphasis on low income families and first-generation college students. Clark never forgot that his business successes began with an engineering scholarship. This has guided the Clark family’s longstanding investments in engineering education and reflects its commitment to ensure college remains accessible and affordable to high-potential students with financial need.
Read the full story at Penn Today. Media contact Evan Lerner and Ali Sundermier.
We are proud to say that three incoming Clark Scholars from the Freshman Class of 2022 will be part of the Bioengineering Department here at Penn.
And finally, our congratulations to the new Dean of the School of Engineering at the University of Mississippi: David A. Puleo, PhD. Dr. Puleo earned his bachelor’s degree and doctorate in Biomedical Engineering from Rensselaer Polytechnic Institute. Most recently he served as Professor of Biomedical Engineering and Associate Dean for Research and Graduate Studies at the University of Kentucky’s College of Engineering. Building on his research in regenerative biomaterials, he also founded Regenera Materials, LLC in 2014. Over the course of his career so far, Dr. Puleo received multiple teaching awards and oversaw much departmental growth within his previous institution, and looks poised to do the same for “Ole Miss.”