A New Treatment for Joint Dysfunction

Medical researchers have long been baffled by the need to find safe and effective treatment for a common condition called temporomandibular joint dysfunction (TMD). Affecting around twenty-five percent of the adult population worldwide, TMD appears overwhelmingly in adolescent, premenopausal women. Many different factors such as injury, arthritis, or grinding of the teeth can lead to the disintegration of or damage to the temporomandibular joint (TMJ), which leads to TMD, although the root cause is not always clear. A type of temporomandibular disorder, TMD can result in chronic pain in the jaw and ears, create difficulty eating and talking, and even cause occasional locking of the joint, making it difficult to open or close one’s mouth. Surgery is often considered a last resort because the results are often short-lasting or even dangerous.
The state of TMD treatment may change with the publication of a study in Science Translational Medicine. With contributions from researchers at the University of California, Irvine (UCI), UC Davis, and the University of Texas School of Dentistry at Houston, this new study has successfully implanted engineered discs made from rib cartilage cells into a TMJ model. The biological properties of the discs are similar enough to native TMJ cells to more fully reduce further degeneration of the joint as well as potentially pave the way for regeneration of joints with TMD.
Senior author Kyriacos Athanasiou, PhD, Distinguished Professor of Biomedical Engineering at UCI, states the next steps for the team of researchers include a long-term study to ensure ongoing effectiveness and safety of the implants followed by eventual clinical trials. In the long run, this technique may also prove useful and relevant to the treatment of other types of arthritis and joint dysfunction.
Advances in Autism Research
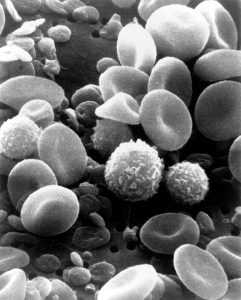
Currently, diagnosis of autism spectrum disorders (ASD) has been limited entirely to clinical observation and examination by medical professionals. This makes the early identification and treatment of ASD difficult as most children cannot be accurately diagnosed until around the age of four, delaying the treatment they might receive. A recent study published in the journal of Bioengineering & Translational Medicine, however, suggests that new blood tests may be able to identify ASD with a high level of accuracy, increasing the early identification that is key to helping autistic children and their families. The researchers, led by Juergen Hahn, PhD, Professor and Department Head of Biomedical Engineering at the Rensselaer Polytechnic Institute, hope that after clinical trials this blood test will become commercially available.
In addition to work that shows methods to detect autism earlier, the most recent issue of Nature Biomedical Engineering includes a study to understand the possible causes of autism and, in turn, develop treatments for the disease. The breakthrough technology of Cas9 enzymes allowed researchers to edit the genome, correcting for symptoms that appeared in mice which resembled autism, including exaggerated and repetitive behaviors. This advance comes from a team at the University of California, Berkeley, which developed the gene-editing technique known as CRISPR-Gold to treat symptoms of ASD by injecting the Cas9 enzyme into the brain without the need for viral delivery. The UC Berkeley researchers suggest in the article’s abstract that these safe gene-editing technologies “may revolutionize the treatment of neurological diseases and the understanding of brain function.” These treatments may have practical benefits for the understanding and treatment of such diverse conditions as addiction and epilepsy as well as ASD.
Penn Professor’s Groundbreaking Bioengineering Technology
Our own D. Kacy Cullen, PhD, was recently featured in Penn Today for his groundbreaking research which has led to the first implantable tissue-engineered brain pathways. This technology could lead to the reversal of certain neurodegenerative disorders, such as Parkinson’s disease.
With three patents, at least eight published papers, $3.3 million in funding, and a productive go with the Penn Center for Innovation’s I-Corps program this past fall, Dr. Cullen is ready to take this project’s findings to the next level with the creation of a brand new startup company: Innervace. “It’s really surreal to think that I’ve been working on this project, this approach, for 10 years now,” he says. “It really was doggedness to just keep pushing in the lab, despite the challenges in getting extramural funding, despite the skepticism of peer reviewers. But we’ve shown that we’re able to do it, and that this is a viable technology.” Several Penn bioengineering students are involved in the research conducted in Dr. Cullen’s lab, including doctoral candidate Laura Struzyna and recent graduate Kate Panzer, who worked in the lab all four years of her undergraduate career.
In addition to his appointment as a Research Associate Professor of Neurosurgery at the Perelman School of Medicine at the University of Pennsylvania, Dr. Cullen also serves as a member of Penn’s Department of Bioengineering Graduate Group Faculty, and will teach the graduate course BE 502 (From Lab to Market Place) for the BE Department this fall 2018 semester. He also serves as the director for the Center of Neurotrauma, Neurodegeneration, and Restoration at the VA Medical Center.
New Prosthetics Will Have the Ability to Feel Pain
New research from the Department of Biomedical Engineering at Johns Hopkins University (JHU) has found a way to address one of the difficult aspects of amputation: the inability for prosthetic limbs to feel. This innovative electronic dermis is worn over the prosthetic, and can detect sensations (such as pain or even a light touch), which are conveyed to the user’s nervous system, closing mimicking skin. The findings of this study were recently published in the journal Science Robotics.
While one might wonder at the value of feeling pain, both researchers and amputees verify that physical sensory reception is important both for the desired realism of the prosthetic or bionic limb, and also to alert the wearer of any potential harm or damage, the same way that heat can remind a person to remove her hand from a hot surface, preventing a potential burn. Professor Nitish Thakor, PhD, and his team hope to make this exciting new technology readily available to amputees.
People and Places
Women are still vastly outnumbered in STEM, making up only twenty percent of the field, and given the need for diversification, researchers, educators, and companies are brainstorming ways to proactively solve this problem by promoting STEM subjects to young women. One current initiative has been spearheaded by GE Healthcare and Milwaukee School of Engineering University (MSOE) who are partnering to give middle school girls access to programs in engineering during their summer break at the MSOE Summer STEM Camp, hoping to reduce the stigma of these subjects for young women. GE Girls also hosts STEM programs with a number of institutions across the U.S.
The National Science Policy Network (NSPN) “works to provide a collaborative resource portal for early-career scientists and engineers involved in science policy, diplomacy, and advocacy.” The NSPN offers platforms and support including grant funding, internships, and competitions. Chaired and led by emerging researchers and professors from around the country, including biomedical engineering PhD student Michaela Rikard of the University of Virginia, the NSPN seeks to provide a network for young scientists in the current political climate in which scientific issues and the very importance of the sciences as a whole are hotly contested and debated by politicians and the public. The NSPN looks to provide a way for scientists to have a voice in policy-making. This new initiative was recently featured in the Scientific American.
Upon its original founding in 2000, the Bill and Melinda Gates Foundation has included the eradication of malaria as part of its mission, pledging around $2 billion to the cause in the years since. One of its most recent initiatives is the funding of a bioengineering project which targets the type of mosquitoes which carry the deadly disease. Engineered mosquitoes (so-called “Friendly Mosquitoes”) would mate in the wild, passing on a mosquito-killing gene to their female offspring (only females bite humans) before they reach maturity. While previous versions of “Friendly Mosquitoes” have been met with success, concerns have been raised about the potential long-term ecological effects to the mosquito population. UK-based partner Oxitec expects to have the new group ready for trials in two years.


 Danielle Bassett, PhD
Danielle Bassett, PhD