Our final Penn Bioengineering seminar of the fall semester will take place this Thursday. Keep an eye on the BE events calendar for upcoming spring seminars.
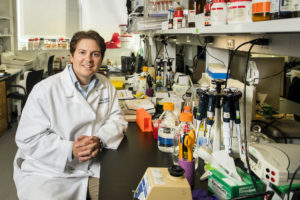
 Speaker: Bijan Pesaran, Ph.D.
Speaker: Bijan Pesaran, Ph.D.
Professor
Neural Science
New York University
Date: Thursday, December 16, 2021
Time: 3:30-4:30 PM EST
Zoom – check email for link
Room: Moore 216
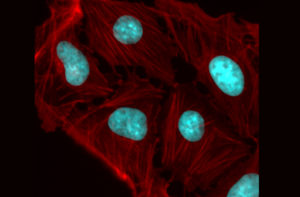
Abstract: Neural engineering is enjoying an era of transformative growth. Classical methods that dominated the neurosciences for decades are being replaced by powerful new technologies. In this talk, I will discuss how to engineer electrical and optical interfaces to the primate brain. I will first present work on electrode interfaces that stimulate and record at the surface of and within the brain. I will show how simultaneously measuring and manipulating neurons immediately beneath electrode contacts during behavior delivers ground-truth data. The results have implications for electrode interface design and new generations of implantable biomedical devices. I will then turn to optical neural interfaces. Two-photon fluorescence microscopy images the activity of neurons expressing genetically-encoded calcium indicators and is most often performed in small animal models, such as the mouse, worm and fly. I will present a cellular-resolution robotic imaging platform to investigate the non-human primate brain at scale. I will finish by discussing potential applications of this technology to a range of scientific and clinical goals.
Bijan Pesaran Bio: Bijan Pesaran is interested in understanding large-scale circuits in the primate brain and how to engineer novel brain-based therapies. Bijan completed his undergraduate degree in Physics at the University of Cambridge, UK. After a year in the Theoretical Physics department at Bell Labs Murray Hill, he went on to earn his PhD in Physics at the California Institute of Technology. He then made the switch to neuroscience as a postdoctoral fellow in Biology at Caltech. Bijan has been on the faculty at New York University since 2006. He is currently a Professor of Neural Science in the Center for Neural Science. In 2013, he was a CV Starr Visiting Scholar at the Princeton Neuroscience Institute at Princeton University. Among other honors and awards, Bijan has received a Burroughs-Wellcome Career Award in the Biomedical Sciences, a Sloan Research Fellowship, a McKnight Scholar Award, the National Science Foundation CAREER Award and is a member of the Simons Collaboration for the Global Brain.