The Department of Bioengineering is proud to announce that five of our faculty have been named on the annual Highly Cited Researchers™ 2021 list from Clarivate:

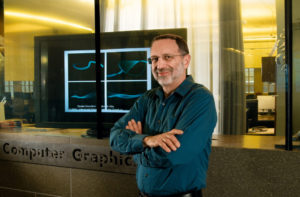
Dani S. Bassett, J. Peter Skirkanich Professor in Bioengineering and in Electrical and Systems Engineering
Bassett runs the Complex Systems lab which tackles problems at the intersection of science, engineering, and medicine using systems-level approaches, exploring fields such as curiosity, dynamic networks in neuroscience, and psychiatric disease. They are a pioneer in the emerging field of network science which combines mathematics, physics, biology and systems engineering to better understand how the overall shape of connections between individual neurons influences cognitive traits.

Jason A. Burdick, Robert D. Bent Professor in Bioengineering
Burdick runs the Polymeric Biomaterials Laboratory which develops polymer networks for fundamental and applied studies with biomedical applications with a specific emphasis on tissue regeneration and drug delivery. The specific targets of his research include: scaffolding for cartilage regeneration, controlling stem cell differentiation through material signals, electrospinning and 3D printing for scaffold fabrication, and injectable hydrogels for therapies after a heart attack.

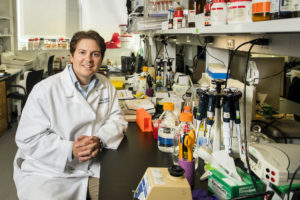
César de la Fuente, Presidential Assistant Professor in Bioengineering and Chemical & Biomedical Engineering in Penn Engineering and in Microbiology and Psychiatry in the Perelman School of Medicine
De la Fuente runs the Machine Biology Group which combines the power of machines and biology to prevent, detect, and treat infectious diseases. He pioneered the development of the first antibiotic designed by a computer with efficacy in animals, designed algorithms for antibiotic discovery, and invented rapid low-cost diagnostics for COVID-19 and other infections.

Carl H. June, Richard W. Vague Professor in Immunotherapy in the Perelman School of Medicine and member of the Bioengineering Graduate Group
June is the Director for the Center for Cellular Immunotherapies and the Parker Institute for Cancer Therapy and runs the June Lab which develops new forms of T cell based therapies. June’s pioneering research in gene therapy led to the FDA approval for CAR T therapy for treating acute lymphoblastic leukemia (ALL), one of the most common childhood cancers.

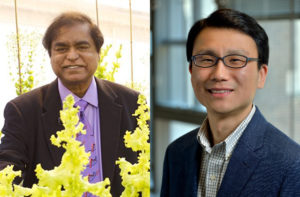
Vivek Shenoy, Eduardo D. Glandt President’s Distinguished Professor in Bioengineering, Mechanical Engineering and Applied Mechanics (MEAM), and in Materials Science and Engineering (MSE)
Shenoy runs the Theoretical Mechanobiology and Materials Lab which develops theoretical concepts and numerical principles for understanding engineering and biological systems. His analytical methods and multiscale modeling techniques gain insight into a myriad of problems in materials science and biomechanics.
The highly anticipated annual list identifies researchers who demonstrated significant influence in their chosen field or fields through the publication of multiple highly cited papers during the last decade. Their names are drawn from the publications that rank in the top 1% by citations for field and publication year in the Web of Science™ citation index.
Bassett and Burdick were both on the Highly Cited Researchers list in 2019 and 2020.
The methodology that determines the “who’s who” of influential researchers draws on the data and analysis performed by bibliometric experts and data scientists at the Institute for Scientific Information™ at Clarivate. It also uses the tallies to identify the countries and research institutions where these scientific elite are based.
David Pendlebury, Senior Citation Analyst at the Institute for Scientific Information at Clarivate, said: “In the race for knowledge, it is human capital that is fundamental and this list identifies and celebrates exceptional individual researchers who are having a great impact on the research community as measured by the rate at which their work is being cited by others.”
The full 2021 Highly Cited Researchers list and executive summary can be found online here.