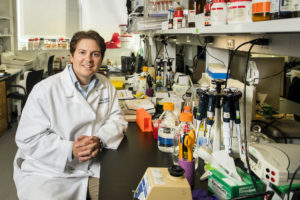
Penn Bioengineering is proud to congratulate Sunghee Estelle Park, Ph.D. on her appointment as Assistant Professor in the Weldon School of Biomedical Engineering at Purdue University. Park earned her Ph.D. at Penn Bioengineering, graduating in July 2023. She conducted doctoral research in the BIOLines Lab of Dan Huh, Associate Professor in Bioengineering. Her appointment at Purdue will begin January 2024.
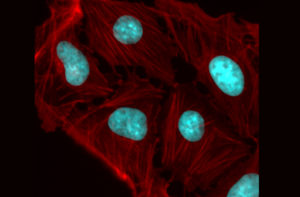
During her Ph.D. research, Park forged a unique path that combined principles in developmental biology, stem cell biology, organoids, and organ-on-a-chip technology to develop innovative in vitro models that can faithfully replicate the pathophysiology of various human diseases. Using a microengineered model of the human retina, she discovered previously unknown roles of the MAPK, IL-17, PI3K-AKT, and TGF-β signaling pathways in the pathogenesis of age-related macular degeneration (AMD), presenting novel therapeutic targets that could be further investigated for the development of AMD treatments. More recently, she tackled a significant challenge in the organoid field, the limited tissue growth and maturity in conventional organoid cultures, by designing microengineered systems that enabled organoids to grow with unprecedented levels of maturity and human-relevance. By integrating these platforms with bioinformatics and computational analyses, she identified novel disease-specific biomarkers of inflammatory bowel disease (IBD) and intestinal fibrosis, including previously unknown link between the presence of lncRNA and the development of IBD.
“The unique interdisciplinary expertise I gained from these projects has shaped me into a scholar with a strong collaborative ethos, a quality I hold in high esteem as we work towards advancing our knowledge and management of health and disease,” says Park.
Her vision as an independent researcher is to become a leading faculty who makes impactful contributions to our fundamental understanding of the factors influencing the structural and functional changes of human organs in health and disease. To achieve this, she plans to lead a stem cell bioengineering laboratory with a primary focus on tissue engineering and regenerative medicine. This will involve developing human organoids-on-a-chip systems and establishing next-generation biomedical devices and therapies tailored for regenerative and personalized medicine.
“I am grateful to all my Ph.D. mentors and lab mates at the BIOLines lab and especially my advisor Dr. Dan Huh, for his exceptional guidance, unwavering support, and invaluable mentorship throughout my Ph.D. journey,” says Park. “Dan’s expertise, dedication, and commitment to excellence have been instrumental in shaping both my research and professional development, while also training me to become an independent scientist and mentor.”
Congratulations to Dr. Park from everyone at Penn Bioengineering!

 David Brainard is the RRL Professor of Psychology, director of the
David Brainard is the RRL Professor of Psychology, director of the