by Erica K. Brockmeier

From smartphones and fitness trackers to social media posts and COVID-19 cases, the past few years have seen an explosion in the amount and types of data that are generated daily. To help make sense of these large, complex datasets, the field of data science has grown, providing methodologies, tools, and perspectives across a wide range of academic disciplines.
But the challenges that lie ahead for data scientists and engineers, from developing algorithms that don’t exacerbate biases to ensuring privacy protections, are equally complex and, in some instances, require entirely new ways of thinking.
As part of its $750 million investment in science, engineering, and medicine, the University has committed to supporting the future needs of this field. To this end, the Innovation in Data Engineering and Science (IDEAS) initiative will help Penn become a leader in developing data-driven approaches that can transform scientific discovery, engineering research, and technological innovation.
“The IDEAS initiative is game-changing for our University,” says President Amy Gutmann. “This new investment allows us to boost our interdisciplinary efforts across campus, recruit phenomenal additional team members, and generate an even more sound foundation for discovery, experimentation, and design. This initiative is a clear statement that Penn is committed to taking data science head-on.”
Building on a foundation of existing expertise
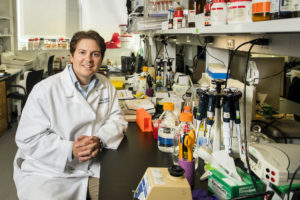
Led by the School of Engineering and Applied Science, the IDEAS initiative builds upon the steadily gathering momentum of its data-centric research. The Warren Center for Network and Data Sciences has been a major catalyst for this type of work, generating foundational research on ethical algorithms and data privacy, as well as collaborations that have drawn in faculty from the Wharton School, Law School, Perelman School of Medicine, and beyond. In addition, Wharton’s Department of Statistics and Data Science is an active partner in research and teaching initiatives that apply statistical modeling across a wide variety of fields.
“One of the unique things about data science and data engineering is that it’s a very horizontal technology, one that is going to be impacting every department on campus,” says George Pappas, Electrical and Systems Engineering Department chair. “When you have a horizontal technology in a competitive area, we have to figure out specific areas where Penn can become a worldwide leader.”
To do this, IDEAS aims to recruit new faculty across three research areas: artificial intelligence (AI) to transform scientific discovery, trustworthy AI for autonomous systems, and understanding connections between the human brain and AI.
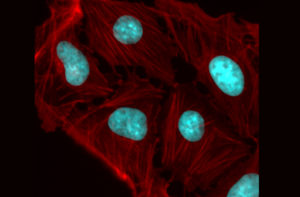
Penn already has a strong foundation in using AI for scientific discovery thanks in part to investments in basic research facilities such as the Singh Center for Nanotechnology and the Laboratory for Research on the Structure of Matter. Additionally, there are centers focused on connecting researchers from different fields to address complex scientific questions, including the Center for Soft and Living Matter, Center for Engineering Mechanobiology, and Penn Institute for Computational Science.
Developing “trustworthy” algorithms, ones that work reliably outside of situations in which they are trained, is another key component of the IDEAS initiative. Ongoing research at the Penn Research in Embedded Computing and Integrated Systems Engineering (PRECISE) Center, the General Robotics, Automation, Sensing & Perception (GRASP) Lab, and DARPA-funded projects on the safety of AI-based aircraft control provide a starting point for furthering Penn’s research portfolio on safe, explainable, and trustworthy autonomous systems.
In the area of neuroscience and how the human brain is similar to AI and machine learning approaches, research from PIK Professor Konrad Kording and Dani Bassett’s Complex Systems lab exemplifies the types of cross-disciplinary efforts that are essential for addressing complex questions. By recruiting additional faculty in this area, IDEAS will help Penn make strides in bio-inspired computing and in future life-changing discoveries that could address cognitive disorders and nervous system diseases.
Read the full story in Penn Today.