Speaker: Audrey Bowden, Ph.D.
Dorothy J. Wingfield Phillips Chancellor’s Faculty Fellow and Associate Professor of Biomedical Engineering and Electrical Engineering & Computer Science
Vanderbilt University
Date: Thursday, November 19, 2020
Time: 3:00-4:00 PM EST
Zoom – check email for link or contact ksas@seas.upenn.edu
Title: “Emerging Technologies for Detection of Early Stage Bladder Cancer”
Abstract:
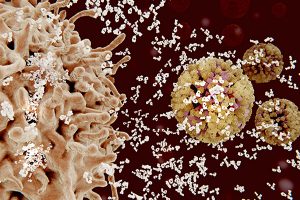
Bladder cancer (BC) — the 4th most common cancer in men and the most expensive cancer to treat over a patient’s lifetime — is a lifelong burden to BC patients and a significant economic burden to the U.S. healthcare system. The high cost of BC stems largely from its high recurrence rate (>50%); hence, BC management involves frequent surveillance. Unfortunately, the current in-office standard-of-care tool for BC surveillance, white light cystoscopy (WLC), is limited by low sensitivity and specificity for carcinoma in situ (CIS), a high-grade carcinoma with high potential to metastasize. Early detection and complete eradication of CIS are critical to improve treatment outcomes and to minimize recurrence. The most promising macroscopic technique to improve sensitivity to CIS detection, blue light cystoscopy (BLC), is costly, time-intensive, has low availability and a high false-positive rate. Given the limitations of WLC, we aim to change the paradigm around how BC surveillance is performed by validating new tools with high sensitivity and specificity for CIS that are appropriate for in-office use. In this seminar, I discuss our innovative solutions to improve mapping the bladder for longitudinal tracking of suspicious lesions and to create miniature tools for optical detection based on optical coherence tomography (OCT). OCT and its functional variant, cross-polarized OCT, can detect early-stage BC with better sensitivity and specificity than WLC. We discuss the critical technical innovations necessary to make OCT and CP-OCT a practical tool for in-office use, and new results from recent explorations of human bladder samples that speak to the promise of this approach to change the management of patient care.
Bio:
Audrey K. Bowden is the Dorothy J. Wingfield Phillips Chancellor Faculty Fellow and Associate Professor of Biomedical Engineering (BME) and of Electrical Engineering and Computer Science (EECS) at Vanderbilt University. Prior to this, she served as Assistant and later Associate Professor of Electrical Engineering and Bioengineering at Stanford University. Dr. Bowden received her BSE in Electrical Engineering from Princeton University, her PhD in BME from Duke University and completed her postdoctoral training in Chemistry and Chemical Biology at Harvard University. During her career, Dr. Bowden served as an International Fellow at Ngee Ann Polytechnic in Singapore. From 2007-2008, she was the Arthur H. Guenther Congressional Fellow sponsored by the OSA and SPIE and served as a Legislative Assistant in the United States Senate through the AAAS Science and Technology Policy Fellows Program. Dr. Bowden is a Fellow of SPIE, a Fellow of AIMBE and is the recipient of numerous awards, including the Air Force Young Investigator Award, the NSF Career Award, the Hellman Faculty Scholars Award, the Phi Beta Kappa Teaching Award, Ford Foundation Postdoctoral Fellowship, and the NSBE Golden Torch Award. She is a former Associate Editor of IEEE Photonics Journal, former Lead Guest Editor of a Biomedical Optics Express Special Issue and is a member of numerous professional committees. Her research interests include biomedical optics – particularly optical coherence tomography and near infrared spectroscopy – microfluidics, and point of care diagnostics.