At the end of April, the graduating seniors in the Penn Department of Bioengineering‘s B.S.E. (Bachelor of Science in Engineering) program presented their Senior Design projects. Developed over the course of their final two semesters in the undergraduate program, these projects are developed in teams of three or four as the students are guided through choosing and understanding an impactful biomedical problem, defining the characteristics of a successful design solution to eliminate or mitigate a problem or fulfill a need, identifying constraints, and creatively developing potential design solutions. Over the course of two days, the students then present their projects to faculty and students from across the Penn Engineering community.
Additionally, three groups (BreatheSmart, RIPT, and Proscopy) were selected to represent BE in the 2019 Penn Engineering Senior Design Project Competition.
Congrats to all of our graduating students on their innovative projects. Check out some photos from the 2019 BE Senior Design presentations and read the full list of this year’s abstracts below.
Group A: BreatheSmart
Caroline Atkinson, Sarah Cai, Rebecca Kellner, Harrison Troché
In the United States, more than 51 million people have been diagnosed with either asthma or chronic obstructive pulmonary disorder (COPD) as of 2016. These conditions result in swelling of the airways, making it difficult to breathe, but the symptoms are commonly managed through the use of a pressurized metered dose inhaler (pMDI), which dispenses aerosolized medication to the lungs, and are currently used by 78% of asthma patients in the US. However, a recent study showed up to 90% of pMDI users incorrectly use their inhalers, reducing the efficacy of medication . Our solution guides patients through the proper technique for using inhalers while providing real-time feedback so patients can correct their technique. This was accomplished by tracking flow rate data converted from a pressure sensor and a smartphone app that provides real-time visual feedback to the user. We were successful in our four design goals as the final device is: (1) lightweight and compact (78 grams with inhaler and 2.5”x1.5”x3.5”), (2) accurate in flow rate measurements (±8.7% error), (3) easy-to-use, with 95% of users surveyed able to use the app successfully without assistance (n=20), and (4) low cost, with the total cost being $76. To improve the design, we will improve accuracy and compactness, and reduce cost. Some ways this could be achieved are through the use of a smaller, custom microcontroller, and a more sensitive pressure sensor. Next steps would include a clinical trial to demonstrate the effectiveness of our device.
Group B: RIPT
Toren Arginteanu, Anna Mujica, Justin Mills, Kayla Prezelski
The tourniquet is the gold standard for treating traumatic extremity bleeding in pre-hospital emergency scenarios. Existing pneumatic tourniquets are safer than non-pneumatic alternatives, minimizing nerve damage and loss of limb function. However, current emergency pneumatic tourniquets are costly and delicate and prone to leaking, punture, and abrasion. Therefore, there is need for an emergency pneumatic tourniquet that is low-cost, highly durable, and easily applied by laypeople. Our design, the Rapidly Inflating Pneumatic Tourniquet (RIPT), consists of an internal bladder made of tough rubber, a durable outer covering made of ballistic nylon, and a pneumatic inflation mechanism involving an inflator valve, pressurized CO 2 cartridge, and pressure relief and regulator valves that maintain a safe and sufficient internal pressure of 250 mmHg. RIPT is tightened around the injured limb and secured with a spring-loaded, automatically locking PLA and aluminum clasp. RIPT’s average application time was 20 ± 0.4 s, which is significantly shorter than that of the Combat Application Tourniquet (CAT): 32 ± 2.9 s. RIPT’s internal bladder pressure reached 250 ± 4.8 mmHg. RIPT packs up to 87.5 in 3 and weighs 18.8 oz. RIPT has comparable circumferential pressure distribution to CAT and superior axial pressure gradient. RIPT’s raw material cost is $65.62. In the future, the clasp mechanism will be modified to improve ease-of-use and minimize size and weight. RIPT will be tested with trauma surgeons at Penn Presbyterian Hospital, and user feedback will indicate ease-of-use and pain of application relative to the CAT.
Group C: Proscopy
Abigail Anmuth, John Forde, Sarah Raizen, Rohit Shinde
Robotically-assisted surgery is a rapidly evolving technology that is expanding the capabilities of surgeons and improving patient outcomes in fields ranging from cardiothoracic surgery to urology. However, as this technology becomes more widely used, there are distinct limitations that impact the safety of surgical maneuvers, largely because of the lack of haptic feedback in the robotic arms of these surgical systems. In the case of prostatectomies, this can lead to the unintentional penetration of the rectal wall and cause pervasive infection, a condition known as rectal injury (RI). Proscopy is a novel real-time proximity sensor that monitors the distance between robotic surgical tools and a patient’s rectal wall to reduce the incidence of RI. This two-part preventative solution consists of a Hall Effect sensor-embedded brace at the tip of the surgical arm and a magnetized flexible insert. The Hall Effect sensors convert magnetic field strength to distance from the rectal wall. In lieu of haptic feedback, Proscopy provides visual feedback within the robot control console as the surgical robot arm nears the rectal wall, displaying information that cannot be perceived from the laparoscopic camera itself. Proscopy gives surgeons the ability to detect the rectal wall with a precision of 0.1±.05mm, rendering it a highly effective and streamlined mechanism for RI prevention during robotically-assisted prostatectomies.
Group D: CerviAid
Dana Abulez, Dayo Adetu, Lamis Elsawah, Yueqi Ren
Cervical insufficiency is premature dilation of the cervix in pregnant women without active labor, and if not addressed, can lead to the loss of pregnancy in the second trimester. This condition results in a protrusion of the amniotic sac out of the uterus and into the cervix, which must be pushed back to extend the pregnancy. In the cervical cerclage procedure, the only treatment for this condition, the cervix is sutured shut to prolong pregnancy. If the cerclage is completed after 14 weeks of pregnancy or if the cervix is more than 3 cm dilated, the procedure is termed an emergency cerclage, which has a higher rate of pregnancy loss due to amniotic sac puncture than regular cerclage procedures. Cerclage procedures are dependent on surgeon experience and utilize no standard method to push back the amniotic sac, which makes this procedure even more high risk. To combat this issue, CerviAid is a device that aims to increase the success rate of emergency cerclages, for which no standardized method exists. The device pushes up the amniotic sac gently with a silicone head and can accommodate a variety of cervix diameters found in patients. The head of the device is controlled by a rack and pinion with a locking mechanism to secure the device and firmly support the sac while the surgeon places the suture. Evaluations of CerviAid with a realistic model of the cervix and amniotic sac produced a 96.15% success rate, in which no membranes were ruptured after pushing through a model cervix. Future steps include further stakeholder evaluations and decreasing manufacturing costs.
Group E: ArcAlert
Kelsey Friberg, Weiwei Meng, Vanessa Moody, Malika Shukurova
Risk of surgical fire increases with use of surgical energy like electrocautery, which presents a source of ignition in an operating room setting with elevated percent oxygen saturation in the air and abundant flammable materials. To address this problem, the FDA recommends human factors strategies, such as heightening awareness, and training on use of surgical energy, which is available yet not standardized across the field. ArcAlert offers a real-time risk management solution for data-driven prevention of surgical fires during use of da Vinci robot electrocautery. The system includes an oxygen sensor device that detects percent oxygen saturation at the surgical field, a machine vision algorithm that detects electrical arcing, and a user-friendly web application. ArcAlert consolidates and assesses risk factor information so that if the oxygen sensor device’s reading exceeds a dangerous threshold or the machine vision algorithm detects arcing, an alert appears on the web application describing the risk, which facilitates improvements to equipment usage by operating room personnel. The oxygen sensor device acquires reliable readings over the timespan of a procedure with an accuracy within +/- 1% for 97% of readings. The machine vision algorithm detects approximately 80% of arcing incidences with only 20% falsely labeled, achieves spatial localization on the order of under 1 centimeter, and executes full pipeline implementation in under half a second. The current design is indicated for transoral surgeries, so future generations will diversify the types of procedures with which the system is compatible, in addition to going fully wireless.
Group F: Grip Glove
Kathryn Khaw, Matthew Rosenwasser, Vidula Kopli
Soft robotics offers many advantages over traditional robotics as an assistive and rehabilitative technology due to its cost-effectiveness and ability to mimic physiological movements. Because of the importance of grip on a patient’s quality of life, we leveraged soft robotic technology to create a flexible, exoskeleton glove for both therapy and assisting daily living for patients with hand impairments. Our device targets muscular dystrophy patients because these patients have a limited selection of devices for their needs. Our design consists of soft robotic actuators attached to a glove that mimic finger movement by bending upon inflation and surface electromyography (SEMG) sensors on the arm to predict the user’s intention to grip or release. Our device effectively recapitulates the forces generated during the grip of a healthy individual using three soft robotic actuators, with each actuator generating 2.83 ± 0.44 N (n = 6). The actuation frequency is 0.2 Hz (12 grips/minute) due to delays in deflation. The EMG sensors, MyoWare and OYMotion Analog EMG Sensor, were not sensitive enough to pick up graded changes in muscle activity, meaning we could only replicate an on-off response through a thresholded spike detection of processed EMG signals in two muscle groups that corresponded to grip and release. Going forward, we will use more sensitive EMG sensors, such as the Biosignalsplux Electromyography Muscle Sensor, increase actuation frequency by actively deflating actuators and include a pressure – solenoid feedback system to have controllable grips.
Group G: SpotOn
Julian Mark, Chase Rapine, Jared Rifkin
In this paper, we discuss SpotOn: a novel bioengineering solution to improving anterior cruciate ligament (ACL) tear recovery. ACL tears are very prevalent injuries and typically take 6-9 months to heal [1]. Physical therapy during recovery is costly and time-intensive, and current knee braces for patients do not provide active support to protect the patient. With SpotOn’s dual-faceted smart mirror and dynamic knee brace technology, patients can begin strengthening the ligament and joint sooner after surgery with less risk of re-injury. When the patient exercises with SpotOn, the smart mirror provides feedback on the patient’s exercise form. If the mirror detects an error, it notifies the user and sends a signal to activate the knee brace and straighten the user’s knee. Key specifications for success include latency of knee brace activation, maximum supported load by the brace, and total cost. Latency and cost met specification goals with a delay less than 0.1s (target under 3s) and total cost of $343.25 (target under $600), but maximum torque output of 18.26ft-lbs was short of the 101.25ft-lbs load goal. Future directions for our design include tracking additional metrics besides squat form, increasing maximum torque output of the knee brace, and lastly adding an on-board battery to the brace to improve portability. Our product was not tested clinically, so the next step to implement our solution would be to reach out to clinicians who are treating injured patients and move forward with gathering clinical data.
Group H: TBx
Daphne Cheung, Gabriel Koo, Shelly Teng, Ethan Zhao
Caused by bacterial strain Mycobacterium tuberculosis, tuberculosis (TB) remains one of the world’s deadliest diseases, with over 10 million new cases and 1.3 million deaths in 2017. Currently, the gold standard for TB diagnosis is to sequence a patient sputum sample using a PCR machine called the GeneXpert. Although this method demonstrates high sensitivity and specificity, it is not ideal in low-income developing countries because it is too expensive and inaccessible, priced at $32,000 for equipment, and $17/test. Thus, diagnosis is most widely determined through smear microscopy. However, this method shows low sensitivity and specificity at only 60% and 81%, respectively. Our solution is TBx, a urine-based diagnostic protocol that offers greater diagnostic power than smear microscopy, while maintaining affordability at only a fraction of the price of the GeneXpert. TBx detects the presence of lipoarabinomannan (LAM) in urine, a glycolipid that is specific to active TB cases. Under TBx protocol, LAM is tagged using photoacoustic dye (IR Dye 800CW) and immunoprecipitation beads via anti-LAM antibodies. Samples are then spun down using a centrifuge to wash out excess dye, concentrated by resuspension in only 5mL 1x PBS, and imaged in a 96-well plate. The photoacoustic dye thermally expands and produces photoacoustic signal in response to photoexcitation at λ = 800nm. Compared to smear microscopy, TBx has higher sensitivity (67%, n = 31) and specificity (92%, n = 31). TBx also only costs $1,500 in equipment, and around $12/test. With further refinements to the TBx protocol and point-of-care packaging, TBx shows promise in developing countries to improve the TB diagnosis landscape, especially with its combination of increased sensitivity and specificity, as well as affordability.
Group I: Sensei “The Cast Master”
Carolina Ferrari, Kristen Ho, Blake Thomas, Alfredo Tovar
Acute compartment syndrome (ACS) occurs in 26,500 people in the US each year and is a result of capillary blood flow becoming compromised when tissue pressure exceeds 30 mmHg. The consequences of ACS are extremely severe if it is not immediately diagnosed. ACS can result in permanent muscle damage, nerve damage and/or amputation, and 70% of cases can be traced back to fractures. The current diagnostic method requires invasive pressure measurements if a patient’s primary symptom assessment is inconclusive. Thus, we have designed SENSEI, a non-invasive device that constantly monitors pressure and can diagnose ACS underneath a cast post-fracture. The device interacts with an Android application via bluetooth to let the user know if they are at risk in real time. SENSEI currently measures compartmental pressure of the forearm within a range of 20-40 mmHg with 91% accuracy. In the future, we plan on improving our pressure sensors so that SENSEI can diagnose ACS with 100% confidence. Other potential additions to SENSEI include designing a sleeve for the lower leg and developing an iOS application to capture more market share.
Group J: UrineLuck: Artificial Urinary Sphincter
Jason Grosz, Richard Adamovich-Zeitlin, Teddy Wang, Sally Pennacchi
Urinary incontinence (UI) is a debilitating ailment that impacts the lives of millions of men. Caused by urinary sphincter damage, prostate issues, or overactive bladder muscles, UI can render men homebound and ruin their social and professional lives. The current gold standard intervention for severe UI is the AMS 800, which consists of a pressure regulated cuff surrounding the urethra and a manual pump in the scrotum. The AMS 800 requires an invasive surgery for implantation and is extremely expensive – around $37,000 for the device, surgery, and hospital stay. It also suffers from a high failure rate, around 33% within three years, due to infections, mechanical failures, and tissue atrophy from the cuff blocking perfusion. In this paper, we fabricate and validate a silicone endourethral valve to treat UI in a less expensive, less invasive, and user-friendly way. These valves are inserted into the penile urethra and mimic the mechanics of bite valves commonly found in water bottles, whereby force applied perpendicularly to a slit enables flow. They are cheap, around $0.08 per device in material costs, do not occlude blood perfusion, and can be inserted at home or in an outpatient clinic with a catheter. Through validation in a PDMS model that recapitulates penile mechanics and geometry, we demonstrated that these valves enable strong flow, 4.99 mL/s, minimal leakage, 0.43 drops, and resistance to cyclic stress. With further cytotoxicity and biofilm testing and insertion protocol development, we hope that this design can improve quality-of-life and prognoses for incontinent men.
Group K: Automated Pathology
Olivia Lang, Joseph Maggiore, Prithvi Pendekanti, Olivia Teter
Clinical and laboratory staining protocols are typically an inefficient use of money, resources and manhours. The highly repetitive and standardized nature of this work poses an opportunity for automation. An automated system would allow a physician or clinician the ability to dedicate their time elsewhere, use less staining fluid, and potentially save on thousands of dollars when compared to similar alternatives. Hemauto is an automated diagnostic device as a proof of concept for a lowcost instrument that combines staining, image acquisition, and image analysis capabilities. Hemauto’s first use case is the detection of Malaria. Malaria, despite being highly treatable, is currently an epidemic in African lowresource regions, disproportionately affecting children. The high incidence rate can be attributed to a lack of standardized and effective earlydetection methods. Providing a lowcost, highthroughput device capable of giving a quantitative diagnosis with limited userinput is critical for these regions because current detection methods are either too hightech, not accurate enough, or are too expensive to be administered frequently. Hemauto’s solution synchronizes the actions of motors and computer technology to deliver a diagnosis. It uses two axes of motion controlled by independent stepper motors to follow the standard Giemsa staining protocol. The stained slide is then automatically focused and imaged in front of a 100x objective lens, where the captured images are analyzed to provide a quantified diagnosis. This proof of concept offers incredible promise for future automated pathology devices across many disease areas.
Group L: Preventear
Matt Riley, Jasmine Wang, Mary Zhuo Ke
Adolescent female athletes are at a high risk of Anterior Cruciate Ligament (ACL) tears as a result of improper form and training techniques. ACL tear prevention training programs are designed to reduce one’s future risk of a tear, but these programs are expensive and not available everywhere. PREVENTEAR is our proposed solution. PREVENTEAR is a self-guided jump training system involving a wearable sock and companion mobile app that like a personal trainer, provides instantaneous feedback on your technique, but is inexpensive and portable. The three main parameters important to jump training are knee angle, knee-to-knee distance, and foot landing technique. The ideal form is to have a knee angle between 30 and 90 degrees with respect to the vertical, have a knee-to-knee distance of greater than 60% with respect to hip width, and land on the ball of the foot before the heel. PREVENTEAR uses bluetooth to communicate with the sensors woven into the sock to a phone app and aims to give feedback on the quality of an athlete’s jump as accurately as ACL tear prevention training programs like Sportsmetrics. The app-reported feedback was compared to true values measured by an observer, phone application, and measuring tools to evaluate performance. PREVENTEAR overall provides a means for ACL tear prevention training by being portable and low cost in comparison to Sportsmetrics, and flexible for adolescent female athletes of varying sizes. PREVENTEAR hopes to further improve accuracy and expand to other forms of training important in reducing risk of ACL injury such as strength, flexibility, and plyometric training in the future.
Group M: Autonomous Home Urinalysis
Saumeel Desai, Anand Prabhu, Eshwar Inapuri
Urinalysis is a crucial diagnostic component of managing heart failure, kidney failure, pre-eclampsia and several other medical conditions. Urinalysis currently requires patient willingness, effort, time and money as patients must travel to a lab, wait for results and rely on caregiver support in order to comply with required follow-ups. Current at-home alternatives, such as dipsticks, lack proper controls and cannot reliably be used by physicians to guide therapy. Moreover, patients are opposed to handling urine, leading to low adherence rates. The goal of this design project was to create an autonomous home urinalysis device that greatly reduces the barriers to diagnostic data collection, enabling detection of deterioration and guidance of therapy with higher efficiency. To meet this goal, the proposed design needed to be affordable, fit on top of a toilet tank, take three or fewer simple steps to use and be capable of rapidly and quantitatively measuring urine volume as well as creatinine, sodium, glucose and albumin concentrations in published clinical reference ranges with a coefficient of variance less than 5%. The solution developed can perform urinalysis within two minutes with only three user steps and is quantitative, controlling assay conditions such as light, volume and time. Each of the initial design requirements have been met, but there is still room for improvement in reducing variation, improving usability and design for manufacturing. This work is a successful starting point upon which future iterations can build to successfully meet patient and provider needs in the urinalysis space.
Group N: BubbleBed
Eden Harris, Candace Jasper, Faith Taliaferro, Sandy Tang
Each year, the U.S. healthcare system spends over $11 billion towards the treatment of pressure ulcer. While pressure ulcers commonly occur in long-term care facilities, they are also prevalent in hospitals, with 700,000 patients admitted to U.S. acute care hospitals developing pressure ulcers each year [1]. The current Braden diagnostic questionnaire assesses risk of ulcers development but fails quantify their locations without nurses having to inspect and rotate patients every two hours. Expensive sensing mats exist, but they offer no pressure relief, and smart-feedback beds offer no information about patient bodily pressure. Thus, we combine pressure sensing capabilities with smart feedback technology [2]. We have developed Bubblebed: a mattress-like device capable of visualizing the user’s bodily pressure as well as responding to areas in need of pressure alleviation, as a means of preventing pressure ulcer development. This device increases or decreases pressure in a specified air cushion (or air cell) based on pressure readings received every ten minutes, actuating until all air cells are restored to safe values, the latter of which was drawn from empirical studies [3]. Our final prototype consists of four air cells controlled by an Arduino algorithm that reads in pressure values within the air cell and opens the corresponding valve to either inflate or deflate a given cell. This prototype serves as a proof-of-concept, demonstrating the efficacy of our pressure-sensing feedback loop and workflow. Future clinical applications would necessitate expanding this to a full hospital bed-size mattress overlay with an associated monitor to visualize pressure ulcer risk.


 Some medical conditions, like diabetes or limb amputation, have the potential to result in wounds that never heal, affecting patients for the rest of their lives. Though normal wound-healing processes are relatively understood by medical professionals, the complications that can lead to chronic non-healing wounds are often varied and complex, creating a gap in successful treatments. But biomedical engineering faculty from the University of Connecticut want to change that.
Some medical conditions, like diabetes or limb amputation, have the potential to result in wounds that never heal, affecting patients for the rest of their lives. Though normal wound-healing processes are relatively understood by medical professionals, the complications that can lead to chronic non-healing wounds are often varied and complex, creating a gap in successful treatments. But biomedical engineering faculty from the University of Connecticut want to change that. In response to the unprecedented challenges presented by the global outbreak of the novel coronavirus SARS-CoV-2,
In response to the unprecedented challenges presented by the global outbreak of the novel coronavirus SARS-CoV-2, 







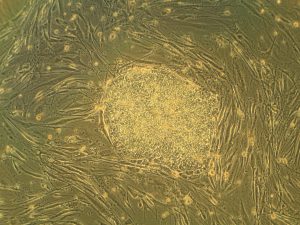 Heart attacks are the result of a stoppage of blood flow to the heart – an interruption to normal function that can result in severe tissue damage, or even tissue death. This loss of healthy tissue function is one of the biggest challenges in treating patients that undergo heart attacks, as the damaged tissue increases their risk of having future attacks. One of the main solutions to this issue right now is the creation of cardiac tissue scaffolds using stem cells to create a platform for new and healthy tissue to grow in vivo. A group of biomedical engineers at Michigan Technological University hopes to
Heart attacks are the result of a stoppage of blood flow to the heart – an interruption to normal function that can result in severe tissue damage, or even tissue death. This loss of healthy tissue function is one of the biggest challenges in treating patients that undergo heart attacks, as the damaged tissue increases their risk of having future attacks. One of the main solutions to this issue right now is the creation of cardiac tissue scaffolds using stem cells to create a platform for new and healthy tissue to grow in vivo. A group of biomedical engineers at Michigan Technological University hopes to 
 Preeclampsia is potentially life-threatening pregnancy disorder that typically occurs in about 200,000 expectant mothers every year. With symptoms of high blood pressure, swelling of the hands and feet, and protein presence in urine, preeclampsia is usually treatable if diagnosed early enough. However, current methods for diagnosis involve invasive procedures like cordocentesis, a procedure which takes a sample of fetal blood.
Preeclampsia is potentially life-threatening pregnancy disorder that typically occurs in about 200,000 expectant mothers every year. With symptoms of high blood pressure, swelling of the hands and feet, and protein presence in urine, preeclampsia is usually treatable if diagnosed early enough. However, current methods for diagnosis involve invasive procedures like cordocentesis, a procedure which takes a sample of fetal blood.