by Melissa Pappas
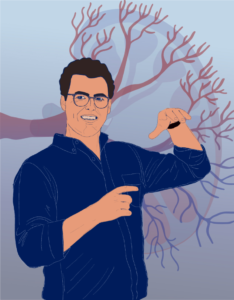
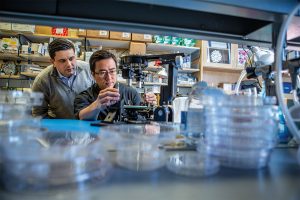
The National Science Foundation’s CAREER Award is given to early-career researchers in order to kickstart their careers in innovative and pivotal research while giving back to the community in the form of outreach and education. Alex Hughes, Assistant Professor in Bioengineering and in Cell and Developmental Biology, is among the Penn Engineering faculty members who have received the CAREER Award this year.
Hughes plans to use the funds to develop a human kidney model to better understand how the development of cells and tissues influences congenital diseases of the kidney and urinary tract.
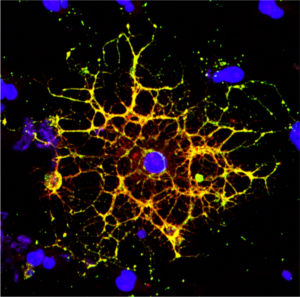
The model, known as an “organoid,” is a lab-grown piece of human kidney tissue on the scale of millimeters to centimeters, grown from cultured human cells.
“We want to create a human organoid structure that has nephrons, the filters of the kidney, that are properly ‘plumbed’ or connected to the ureteric epithelium, the tubules that direct urine towards the bladder,” says Hughes. “To achieve that, we have to first understand how to guide the formation of the ureteric tubule networks, and then stimulate early nephrons to fuse with those networks. In the end, the structures will look like ‘kidney subunits’ that could potentially be injected and fused to existing kidneys.”
The field of bioengineering has touched on questions similar to those posed by Hughes, focusing on drug testing and disease treatment. Some of these questions can be answered with the “organ-on-a-chip” approach, while others need an even more realistic model of the organ. The fundamentals of kidney development and questions such as “how does the development of nephrons affect congenital kidney and urinary tract anomalies?” require an organoid in an environment as similar to the human body as possible.
“We decided to start with the kidney for a few reasons,” says Hughes. “First, because its development is a beautiful process; the tubule growth is similar to that of a tree, splitting into branches. It’s a complex yet understudied organ that hosts incredibly common developmental defects.
“Second,” he says, “the question of how things form and develop in the kidney has major medical implications, and we cannot answer that with the ‘organ-on-a-chip’ approach. We need to create a model that mimics the chemical and mechanical properties of the kidney to watch these tissues develop.”
The fundamental development of the kidney can also answer other questions related to efficiency and the evolution of this biological filtration system.
“We have the tendency to believe that systems in the human body are the most evolved and thus the most efficient, but that is not necessarily true,” says Hughes. “If we can better understand the development of a system, such as the kidney, then we may be able to make the system better.”
Hughes’ kidney research will lay the foundation for broader goals within regenerative medicine and organ transplantation.
Read the full story in Penn Engineering Today.

 NextUp, a regular feature of Philadelphia Magazine that “highlights the local leaders, organizations and research shaping the Greater Philadelphia region’s life sciences ecosystem,” ran a profile of Philly-based agricultural startup Strella Biotechnology. Founded by Penn alumna Katherine Sizov (Bio 2019) and winner of a 2019 President’s Innovation Prize, Strella Biotech seeks to reduce food waste through innovative biosensors, and was initially developed in the
NextUp, a regular feature of Philadelphia Magazine that “highlights the local leaders, organizations and research shaping the Greater Philadelphia region’s life sciences ecosystem,” ran a profile of Philly-based agricultural startup Strella Biotechnology. Founded by Penn alumna Katherine Sizov (Bio 2019) and winner of a 2019 President’s Innovation Prize, Strella Biotech seeks to reduce food waste through innovative biosensors, and was initially developed in the 




 New research from
New research from