by Kaila Helm, Biological Basis of Behavior ’20; Kathleen Givan, Bioengineering and Political Science, ’20; Kathryn Cocherl, Bioengineering ’20; Hope McMahon, Chemical and Biomolecular Engineering ’18; and Dave Pontoriero, Biotechnology MS ’18
David Issadore, a faculty member in the Department of Bioengineering at the University of Pennsylvania teaches an engineering course ENGR566 – Appropriate Point of Care Diagnostics. As part of this course, he and Miriam Wattenberger from CBE, have taken nine Penn students, most of them majoring in Bioengineering, to Kumasi, Ghana, to study the diagnosis of pediatric tuberculosis. While in Ghana, these students are blogging daily on their experiences.
Our day started early. We woke up for a 7:00 a.m. breakfast of our usual combination of rolls with jam, sausages, omelets, and a beverage. After breakfast, we headed for the bus, where Uncle Ebo (our bus driver) was waiting to take us to a rural hospital about an hour away. We soon arrived at the Agogo Presbyterian Hospital. We were amazed by the organization and structure. At our previous hospital visit, we only saw a TB clinic. Today, we got to see a hospital that served a very different community. After spending some time in an old Presbyterian church, an administrator greeted us to begin our tour. We entered the main atrium, a large waiting room filled with more than a hundred people. We even saw a sheet used to characterize patients’ symptoms — a comprehensive list of numerous traits and experiences. We then continued our tour by entering the various wings and sections affiliated with TB treatment. This provided a wonderful opportunity to see a different side of the hospital’s operations.

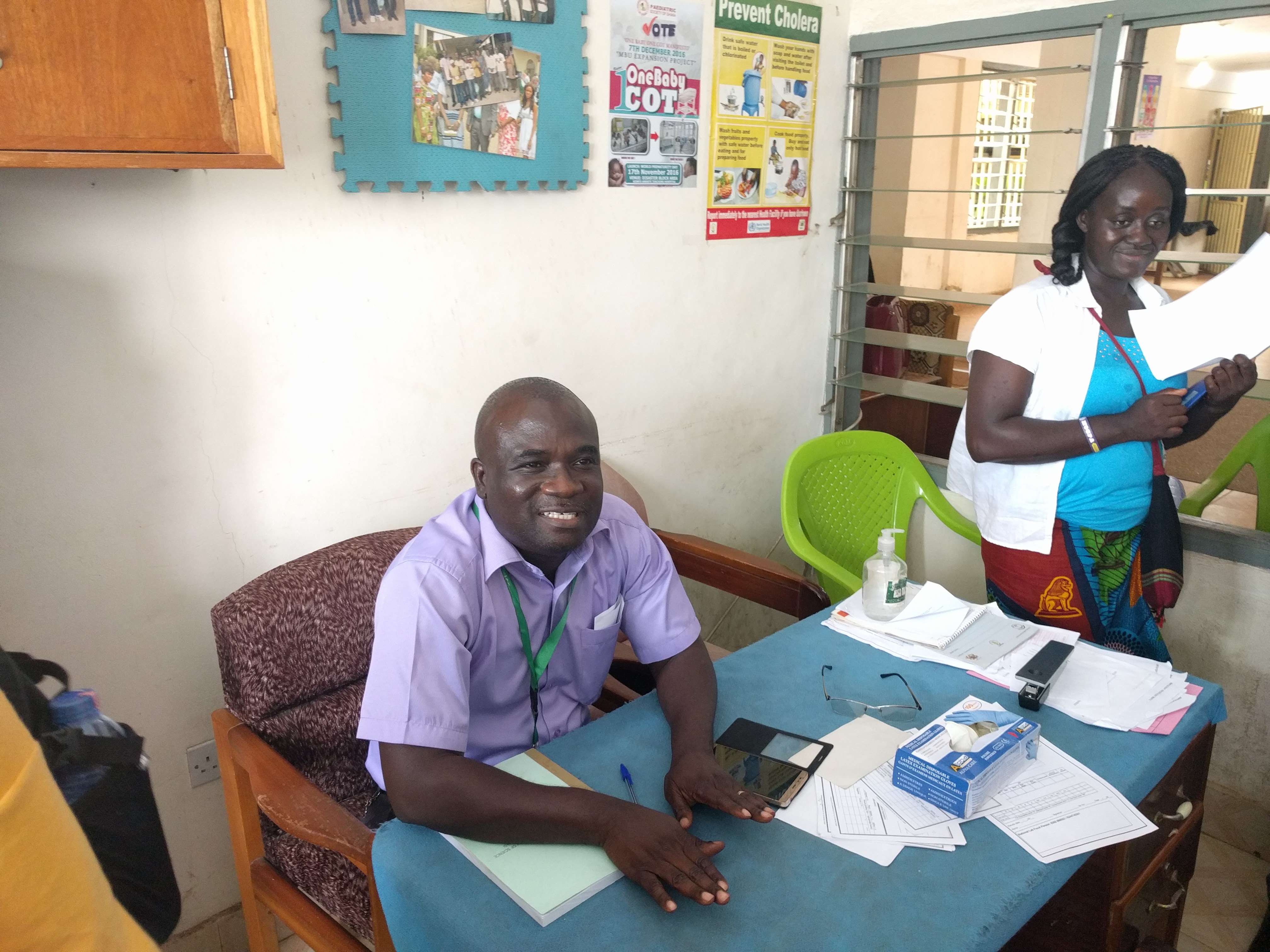
Initially, we were allowed to peek into the diagnosing wing. The first room was small and was purposed for smear microscopy tests. It had a few light microscopes and many technicians. Adjacent to this room was the GeneXpert room. Tucked away in the back corner was a small box (the GeneXpert), maybe 18 inches high. We were surprised at how small and streamlined it was — finally seeing the machine we have talked about for a solid semester was an almost surreal experience. It seems that they value it highly and therefore keep it well maintained and protected. We learned more about how they use the GeneXpert and the limitations they face, such as a limited number of cartridges, problems with overuse, and slow maintenance.
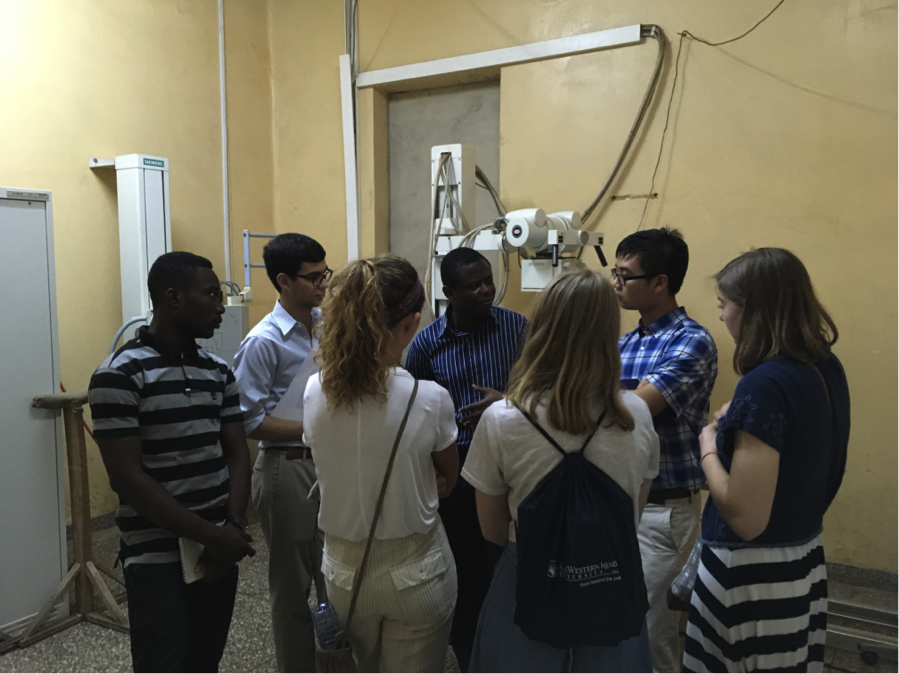
We then went into the X-ray room. As per our past lectures, this is the preferred initial screening methodology, so it was exciting to see how well established their systems are. There were two X-ray machines that were donated and used by the entire facility. The nurse also showed us how they store all the scans and showed us a scan of a pneumonia patient’s lung. They hope to introduce digital X-rays in the future, which will be better for analyzing and diagnosing. She taught us what to look for on the scans, saying that pneumonia is differentiated from TB because it is localized at the bottom lobes of the lung, whereas TB is more widespread and present in the top lobes as well. The tour concluded with a trip to the isolation room for TB patients, but time was limited, so we didn’t spend much time there.
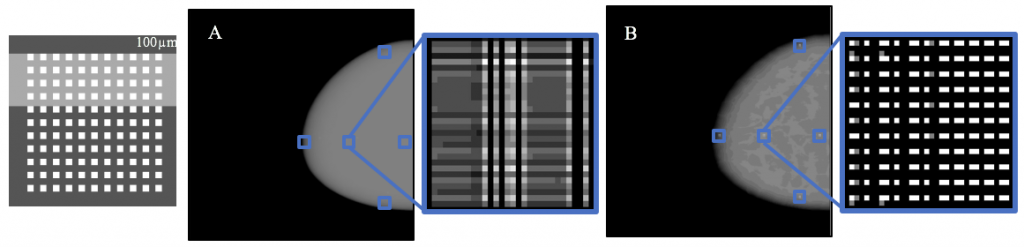
Once we took the bus back to KCCR, we attended a lecture by Dr. David Issadore, who spoke about his research to a packed room filled with Ghanaian clinicians and researchers. They were very interested in his work, especially in how microfluidic chips could be used as a diagnostic for TB. Interestingly, the room was filled with clinicians and research scientists, but engineers were poorly represented. Dr. Issadore definitely made us proud!

(Left to right: Hope McMahon, Salim)
After the presentation, our group scattered. Some of us took control and hand-washed our clothes. A few numb fingers made for a very nice reminder about the little things we take for granted back in the States. After we worked up an appetite, we introduced the American classic of peanut butter and banana sandwiches to the Ghanaian students and Nana. We received some mixed responses, and we won’t be getting many returning customers, but it was nice to have a little bit of role reversal. Considering how much we have learned about Ghanaian culture through their food, it was nice to help them see a little bit of what America has to offer.