by Sophie Burkholder
Synthetic Spinal Discs from a Penn Research Team Might Be the Solution to Chronic Back Pain
Spinal discs, the concentric circles of collagen fiber found between each vertebra of the spine, can be the source of immense back pain when ruptured. Especially for truck and bus drivers, veterans, and cigarette smokers, there is an increased risk in spinal disc rupture due to overuse or deterioration over time. But these patients aren’t alone. In fact, spinal discs erode over time for almost everyone, and are one of the sources of back pain in older patients, especially when the discs erode so much that they allow direct bone-to-bone contact between two or more vertebrae.

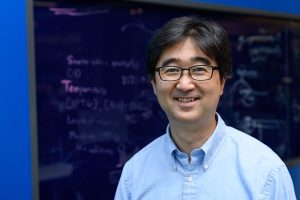
Robert Mauck, Ph.D., who is the director of the McKay Orthopaedic Research Laboratory here at Penn and a member of the Bioengineering Graduate Group Faculty, led a research team in creating artificial spinal discs, with an outer layer made from biodegradable polymer and an inner layer made with a sugar-like gel. Their findings appear in Science Translational Medicine. These synthetic discs are also seeded with stem cells that produce collagen over time, meant to replace the polymer as it degrades in vivo over time. Though Mauck and his time are still far from human clinical trials for the discs, they’ve shown some success in goat models so far. If successful, these biodegradable discs could lead to a solution for back pain that integrates itself into the human body over time, potentially eliminating the need of multiple invasive procedures that current solutions require. Mauck’s work was recently featured in Philly.com.
An Untethered, Light-Activated Electrode for Innovations in Neurostimulation
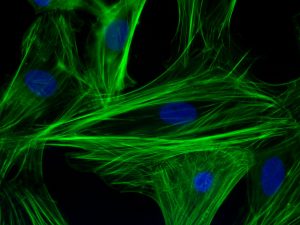
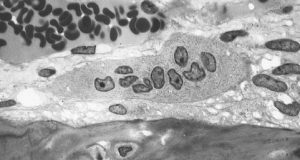
Neurostimulation, a process by which nervous system activity can be purposefully modulated, is a common treatment for patients with some form of paralysis or neurological disorders like Parkinson’s disease. This procedure is typically invasive, and because of the brain’s extreme sensitivity, even the slightest involuntary movement of the cables, electrodes, and other components involved can lead to further brain damage through inflammation and scarring. In an effort to solve this common problem, researchers from the B.I.O.N.I.C. Lab run by Takashi D.Y. Kozai, Ph. D., at the University of Pittsburgh replaced long cables with long wavelength light and a formerly tethered electrode with a smaller, untethered one.
The research team, which includes Pitt senior bioengineering and computer engineering student Kaylene Stocking, centered the device on the principle of the photoelectric effect – a concept first described in a publication by Einstein as the local change in electric potential for an object when hit with a photon. Their design, which includes a 7-8 micron diameter carbon fiber implant, is now patent pending, and Kozai hopes that it will lead to safer and more precise advancements in neurostimulation for patients in the future.
A New Microfluidic Chip Can Detect Cancer in a Drop of Blood
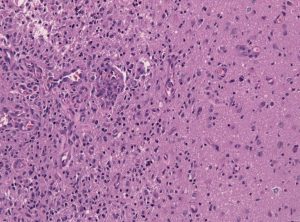
Many forms of cancer cannot be detected until the disease has progressed past the point of optimum treatment time, increasing the risk for patients who receive late diagnoses of these kinds of cancer. But what if the diagnostic process could be simplified and made more efficient so that even a single drop of blood could be enough input to detect the presence of cancer in a patient? Yong Zeng, Ph.D., and his team of researchers at the University of Kansas in Lawrence sought to answer that question.
They designed a self-assembled 3D-nanopatterned microfluidic chip to increase typical microfluidic chip sensitivity so that it can now detect lower levels of tumor-associated exosomes in patient blood plasma. This is in large part due to the nanopatterns in the structure of the chip, which promote mass transfer and increase surface area, which in turn promotes surface-particle interactions in the device. The team applied the device to their studies of ovarian cancer, one of the notoriously more difficult kinds of cancer to detect early on in patients.
A Wearable Respiration Monitor Made from Shrinky Dinks
Michelle Khine, Ph. D., a professor of biomedical engineering at the University of California, Irvine incorporates Shrinky Dinks into her research. After using them once before in a medical device involving microfluidics, her lab recently worked to incorporate them into a wearable respiration monitor – a device that would be useful for patients with asthma, cystic fibrosis, and other chronic pulmonary diseases. The device has the capability to track the rate and volume of its user’s respiration based on measurements of the strain at the locations where the device makes contact with the user’s abdomen.
Paired with Bluetooth technology, this sensor can feed live readings to a smartphone app, giving constant updates to users and doctors, as opposed to the typical pulmonary function test, which only provides information from the time at which the test takes a reading. Though Khine and her team have only tested the device on healthy patients so far, they look forward to testing with patients who have pulmonary disorders, in hopes that the device will provide more comprehensive and accessible data on their respiration.
People and Places
Ashley Kimbel, a high school senior from Grissom High School in Huntsville, Alabama, designed a lightweight prosthetic leg for local Marine, Kendall Bane, after an attack in Afghanistan led him to amputate one of his legs below the knee. Bane, who likes to keep as active as possible, said the new lighter design is more ideal for activities like hiking and mountain biking, especially as any added weight makes balance during these activities more difficult. Kimbel used a CAD-modeling software produced by Siemens called Solid Edge, which the company hopes to continue improving in accessibility so that more students can start projects like Kimbel’s.
This week, we would like to congratulate Angela Belcher, Ph.D., on being named the new head of the Department of Biological Engineering at the Massachusetts Institute of Technology (MIT). With her appointment to this role, now half of the MIT engineering department heads are women. Belcher’s research is in the overlap of materials science and biological engineering, with a particular focus on creating nanostructures based on the evolution of ancient organisms for applications in medical diagnostics, batteries, solar cells, and more.
We would also like to congratulate Eva Dyer, Ph.D., and Chethan Pandarinath, Ph.D., both of whom are faculty members at the Walter H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University, on receiving research fellowships from the Alfred P. Sloan Foundation. Dr. Dyer, who formerly worked with Penn bioengineering faculty member Dr. Konrad Kording while he was at Northwestern University, leads research in the field of using data analysis methods to quantify neuroanatomy. Dr. Pandarinth leads the Emory and Georgia Tech Systems Neural Engineering Lab, where he works with a team of researchers to use properties of artificial intelligence and machine learning to better understand large neural networks in the brain.