by Meagan Raeke

In popular culture, scientific discovery is often portrayed in “Eureka!” moments of sudden realization: a lightbulb moment, coming sometimes by accident. But in real life—and in Penn Medicine’s rich history as a scientific innovator for more than 250 years—scientific breakthroughs can never truly be distilled down to a single, “ah-ha” moment. They’re the result of years of hard work, perseverance, and determination to keep going, despite repeated, often discouraging, barriers and setbacks.
“Research is [like taking], four, or six, or eight steps back, and then a little stumble forward,” said Drew Weissman, MD, PhD, the Roberts Family Professor of Vaccine Research. “You keep doing that over and over and somehow, rarely, you can get to the top of the step.”
For Weissman and his research partner, Katalin Karikó, PhD, an adjunct professor of Neurosurgery, that persistence—documented in thousands of news stories across the globe—led to the mRNA technology that enabled two lifesaving COVID-19 vaccines, earning the duo numerous accolades, including the highest scientific honor, the 2023 Nobel Prize in Medicine.
Weissman and Karikó were also the 2022 recipients of the Breakthrough Prize in Life Sciences, the world’s largest science awards, popularly known as the “Oscars of Science.” Founded in 2012 by a group of web and tech luminaries including Google co-founder Sergey Brin and Meta CEO Mark Zuckerberg, the Breakthrough Prizes recognize “the world’s top scientists working in the fundamental sciences—the disciplines that ask the biggest questions and find the deepest explanations.” With six total winners, including four from the Perelman School of Medicine (PSOM), Penn stands alongside Harvard and MIT as the institutions whose researchers have been honored with the most Breakthrough Prizes.
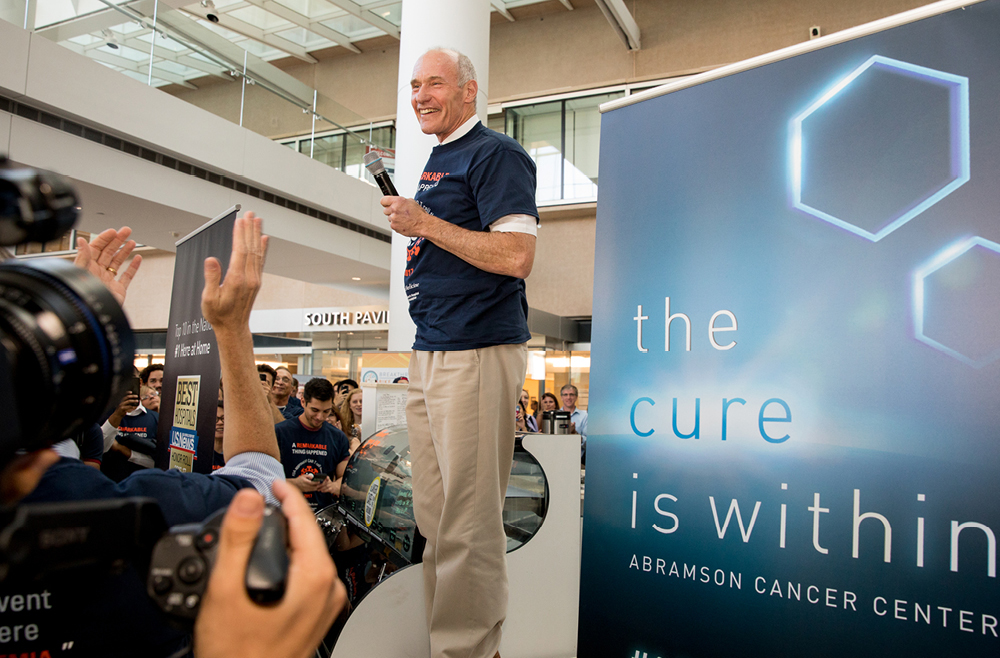
Virginia M.–Y. Lee, PhD, the John H. Ware 3rd Professor in Alzheimer’s Research, was awarded the Prize in 2020 for discovering how different forms of misfolded proteins can move from cell to cell and lead to neurodegenerative disease progression. Carl June, MD, the Richard W. Vague Professor in Immunotherapy, is the most recent recipient and will be recognized at a star-studded red-carpet event in April for pioneering the development of CAR T cell therapy, which programs patients’ own immune cells to fight their cancer.
The four PSOM Breakthrough Prize recipients were honored on Tuesday, Feb. 13, 2024, when a new large-scale installation was unveiled in the lobby of the Biomedical Research Building to celebrate each laurate and their life-changing discoveries. During a light-hearted panel discussion, the honorees shared how a clear purpose, dogged determination, and a good sense of humor enabled their momentum forward.
Read the full story in Penn Medicine News.
Carl June and Jon Epstein are members of the Penn Bioengineering Graduate Group. Read more stories featuring them in the BE Blog here and here, respectively.
Weissman presented the Department of Bioengineering’s 2022 Herman P. Schwan Distinguished Lecture: “Nucleoside-modified mRNA-LNP therapeutics.” Read more stories featuring Weissman in the BE Blog here.