Breast cancer continues to affect more than 10% of all women — and a small percentage of men — despite significant advances in diagnosis and treatment. While a majority cases today can be successfully treated, early detection is essential to beginning treatment before it’s too late.
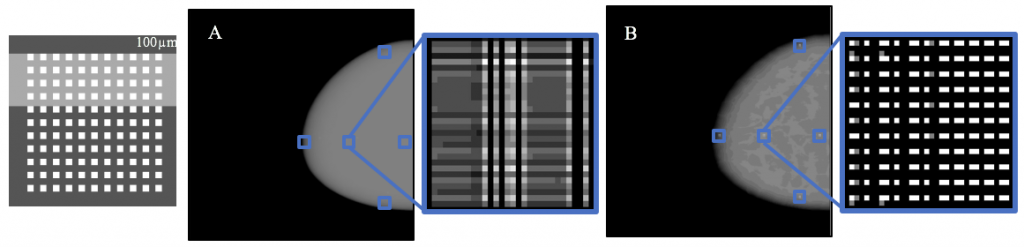
Among the more recent innovations in screening has been three-dimensional mammography. However, this modality has lacked the ability to personalize the scan to the individual patient’s breast, instead only acquiring several two-dimensional images along the chest wall, resulting in a lack of individualization for the patient.
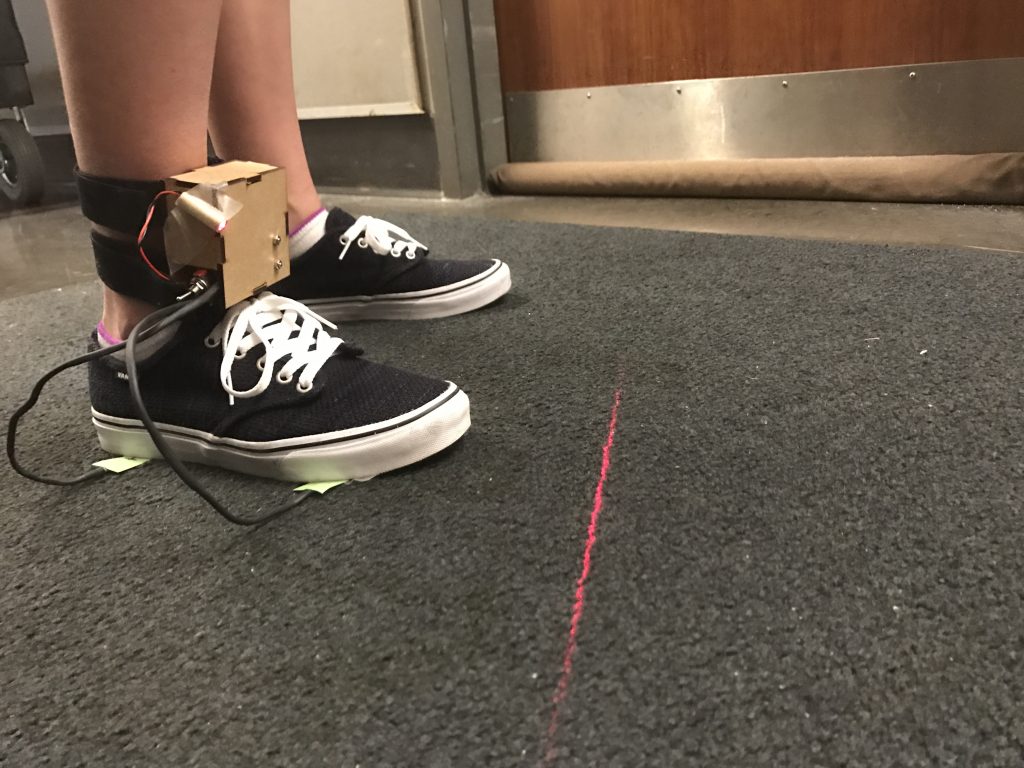
A senior design project team at the University of Pennsylvania’s Department of Bioengineering, however, has helped to develop a more personalized 3D imaging technology, which acquires a series of images but instead following the contour of the breast itself. With their efforts, the team earned one of the three awards given to student teams yearly.
The four-student team, consisting of Lucy Chai, Elizabeth Kobe, Margaret Nolan, and Sushmitha Yarrabothula, picked up a project begun last year (a common practice with senior design projects) and demonstrated with their work that the imaging technique could be applied using a digital phantom (a computerized breast model) with great clarity, including successful resolution of a simulated mass just one-tenth of a millimeter in size.
Now, the four seniors will hand off the project to another team, continuing this multi-year research. Ultimately, before it can be applied in actual patients, the modality will need to be tested against the current standard of care in terms of its ability to detect small masses in the breast. Nevertheless, this year’s team moved the ball downfield significantly.