Imagine a scenario where a skilled hacker must upload critical software to update a central server and thwart a potentially lethal virus from wreaking havoc across a vast computer network. The programmer, armed with the lifesaving code, must navigate through treacherous territory teeming with adversaries, and success hinges on promptly getting a safe, stealthy delivery vehicle that can place the hacker exactly where they need to be.
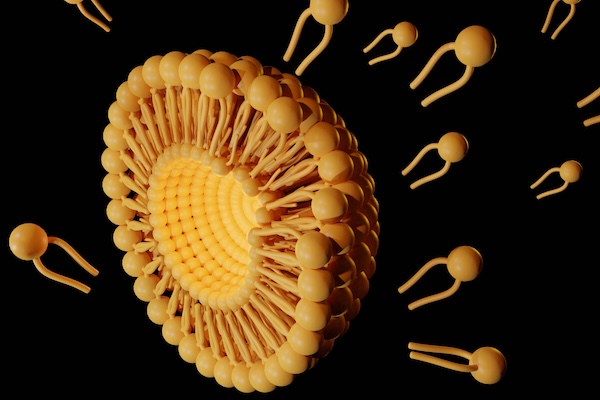
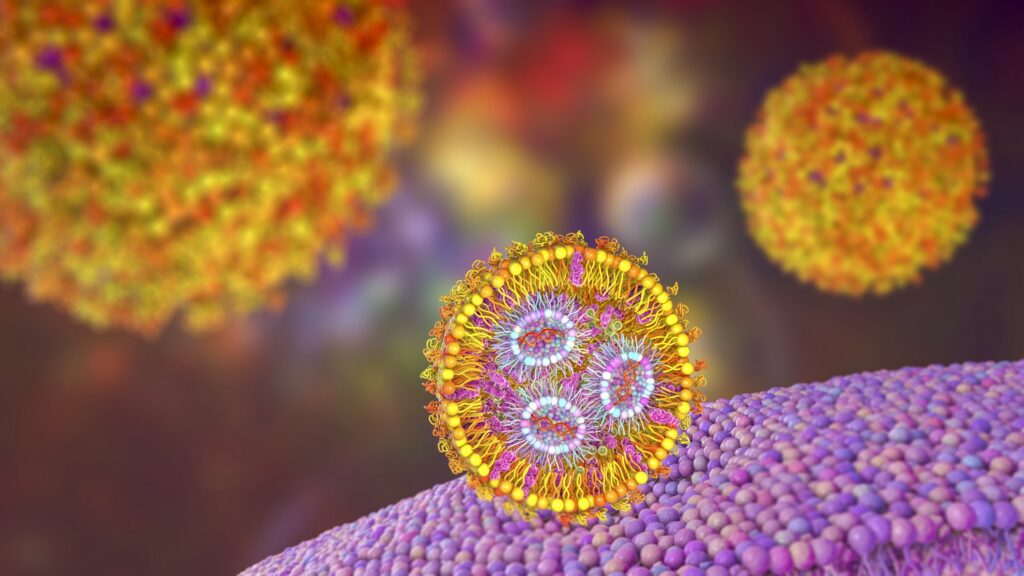
In the context of modern medicine, messenger RNA (mRNA) serves as the hacker, carrying genetic instructions to produce specific proteins within cells that can induce desired immune responses or sequester maladaptive cellular elements. Lipid nanoparticles (LNPs) are the stealthy delivery vehicles that transport these fragile mRNA molecules through the bloodstream to their target cells, overcoming the body’s defenses to deliver their payload safely and efficiently.
However, much like building an advanced stealth vehicle, the synthesis of cationic lipids—a type of lipid molecule that’s positively charged and a key component of LNPs—is often a time-consuming process, involving multiple steps of chemical synthesis and purification.
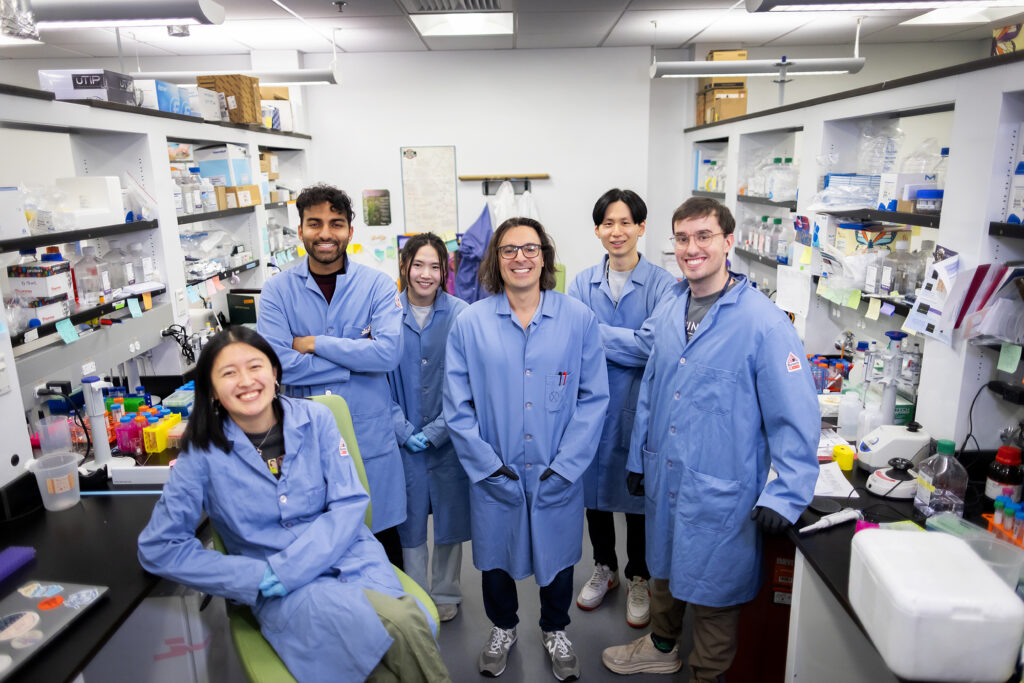
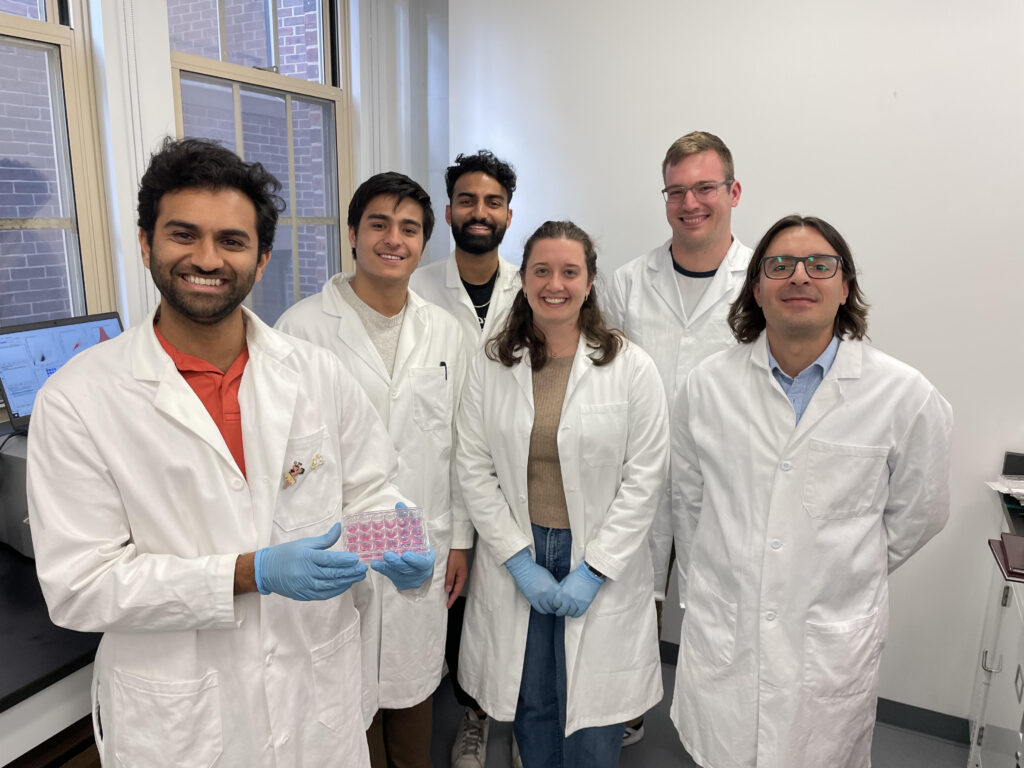
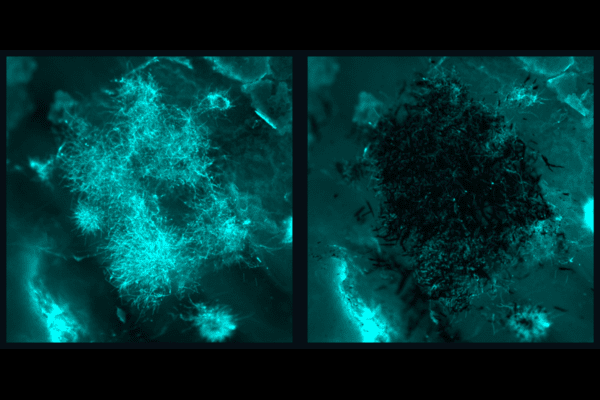
Now, Michael Mitchell and a team at the University of Pennsylvania have addressed this challenge with a novel approach that leverages a compound library fabrication technique known as “click-like chemistry” to create LNPs in a single, simple step. Their findings, published in the journal Nature Chemistry, show that this method not only speeds up the synthesis process but also presents a way to equip these delivery vehicles with a “GPS” to better target specific organs such as the liver, lungs, and spleen, potentially opening new avenues for treating a range of diseases that arise in these organs.
“We’ve developed what we call an amidine-incorporated degradable (AID) lipid, a uniquely structured biodegradable molecule,” Mitchell says. “Think of it as an easy-to-build custom mRNA vehicle with a body kit that informs its navigation system. By adjusting its shape and degradability, we can enhance mRNA delivery into cells in a safe manner. By adjusting the amount of the AID lipid that we incorporate into the LNP, we can also guide it to different organs in the body, much like programming different destinations into a GPS.”
First author Xuexiang Han, a former postdoctoral researcher in the Mitchell Lab, explains that their new approach allows the rapid creation of diverse lipid structures in just an hour, compared to the weekslong process traditionally required.
Read more in Penn Today.