
Kaitlin Mrksich, an undergraduate student in Penn Bioengineering, was honored with the Student Award for Outstanding Research (Undergraduate) by the Society for Biomaterials (SFB). This prestigious award recognizes undergraduate students who have shown outstanding achievement in biomaterials research.
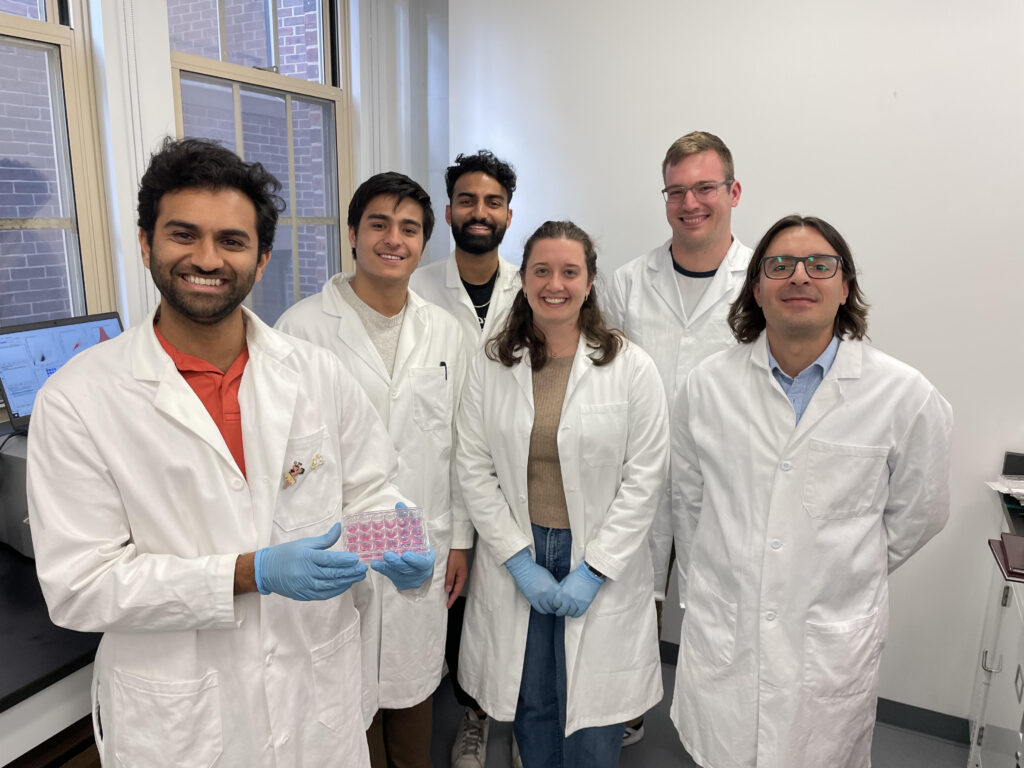
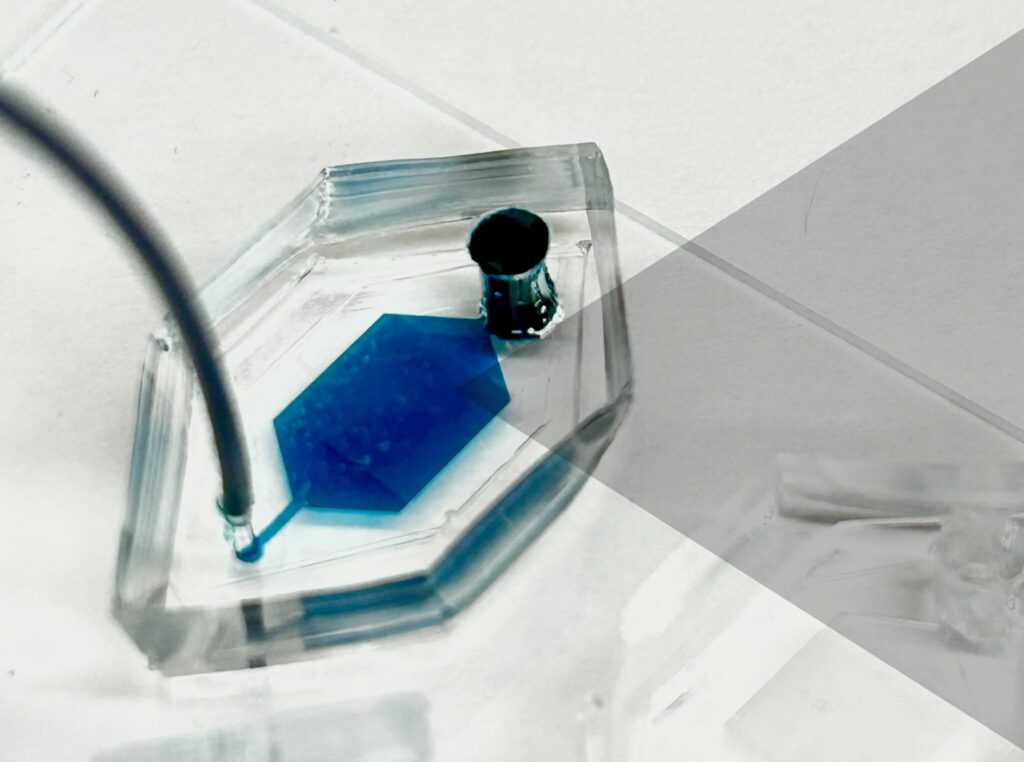
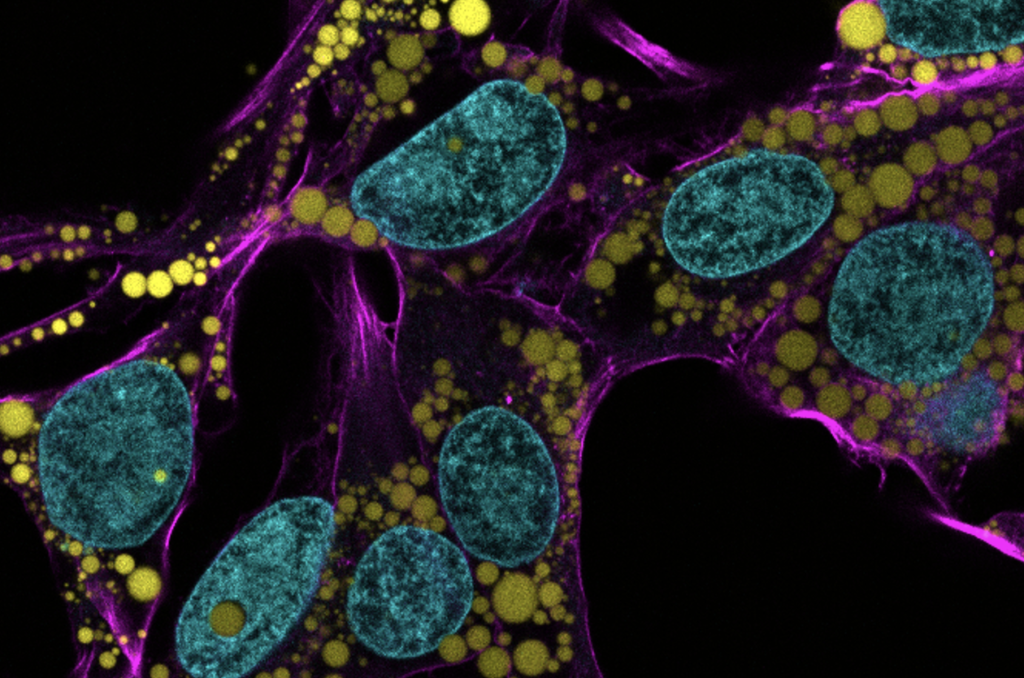
Mrksich is a third-year student from Hinsdale, Illinois. She is interested in developing drug delivery systems that can serve as novel therapeutics for a variety of diseases. She works in the lab of Michael Mitchell, Associate Professor in Bioengineering. In the Mitchell Lab, Mrksich investigates the ionizable lipid component of lipid nanoparticles for mRNA delivery.
“In Kaitlin’s independent projects, she has focused on probing the role of lipophilicity and chirality for LNP-mediated mRNA delivery,” Mitchell said in the award announcement. “She has synthesized dozens of unique lipids, formulated these lipids into LNPs, and evaluated their potential for mRNA delivery in vivo and in primary T cells. She has been able to deduce structure-function relationships that help explain the role of lipid hydrophobicity in the delivery of mRNA by LNPs. Her findings have not only been instrumental in helping our lab design better LNPs but will also provide fundamental knowledge that will benefit all labs working on LNP technology.”
In addition to her academic activities, Mrksich is also the President of the Penn Biomedical Engineering Society (BMES), where she plans community-building and professional-development events for bioengineering majors, and the visit coordinator for special programs for the Kite and Key Society, where she organizes virtual programming to introduce prospective students to Penn. She also tutors a West Philadelphia high school student in chemistry as part of the West Philadelphia Tutoring Project and is a member of Tau Beta Pi engineering honor society and Sigma Kappa sorority. After graduating, she plans to pursue an M.D.-Ph.D. in Bioengineering.
Read the full list of 2024 SFB award recipients here.


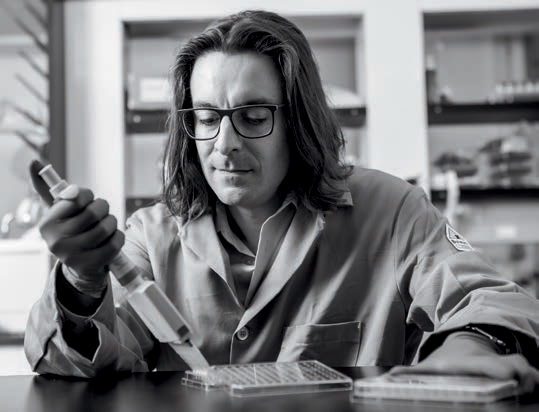

 Cosette Tomita, a master’s student in Bioengineering, spoke with Penn Engineering Graduate Admissions about her research in cellular therapy and her path to Penn Engineering.
Cosette Tomita, a master’s student in Bioengineering, spoke with Penn Engineering Graduate Admissions about her research in cellular therapy and her path to Penn Engineering.