A New Model of the Small Intestine
Diseases of the small intestine, including Crohn’s disease and microbial infections, impose a huge burden on health. However, finding treatments for these diseases is challenged by the lack of optimal models for studying disease. Animal models are only so close to human disease states, and laboratory models using cell lines do not completely mimic the environment inside the gut.
However, these limitations might be overcome soon thanks to the research of scientists at Tufts University. In an article recently published in PLOS ONE, a team led by David L. Kaplan, Ph.D., of the Tufts Department of Biomedical Engineering, describes how they used donor stem cells and a compartmentalized biomimetic scaffold to model and generate small intestine cells that could differentiate into the broad variety of cell types common to that organ.
The study team tested the response of its cell model to E. coli, a common pathogen. At the genetic level, the model matched the reaction of the human small intestine when exposed to this bacterium. The success of the model could translate into its use in the near future to better understand the digestive system’s response to infection, as well as to test individualized treatments for inflammatory bowel diseases such as Crohn’s.
Saving Battle-wounded Eyes
The increase in combat survival rates has led to a higher incidence of veterans with permanent vision loss due to catastrophic damage to the eye. Globe injuries will recover of some vision, if caught in time. However, combat care for eye injuries often occurs hundreds or thousands of miles away from emergency rooms with attending ophthalmologists. With this unavoidable delay in treatment, people with globe injuries suffer blindness and often enucleation.
However, battle medics might soon have something in their arsenals to prevent such blinding injuries immediately in the combat theater. As reported recently in Science Translational Medicine, engineers at the University of Southern California (USC) and ophthalmologists from USC’s Roski Eye Institute have collaborated in creating a new material for temporary sealing of globe injuries. The study authors, led by John J. Whalen, III, Ph.D., used a gel called poly(N-isopropylacrylamide) (PNIPAM), already under investigation for treating retinal injuries. PNIPAM is a thermoresponsive sealant, meaning it is a liquid at cooler temperature but an adhesive gel at warmer temperature. These interesting properties mean PNIPAM can be applied as a liquid and then solidifies quickly on the eye. The authors manipulated PNIPAM chemically to make it more stable at body temperature. As envisioned, the gel, when used with globe injuries, could be applied by medics and then removed with cold water just before the eye is treated.
The study team has tested the gel in rabbits, where it showed statistically significant improvement in wound sealing and no negative effects on the eyes or overall health of the rabbits. The authors believe the material will be ready for human testing in 2019.
Predicting Seizures in Epilepsy
Epilepsy is a central nervous system disorder characterized by seizure activity that can range in severity from mild to debilitating. Many patients with epilepsy experience adequate control of seizures with medications; however, about a third of epileptic patients have intractable cases requiring surgery or other invasive procedures.
In what could be a breakthrough in the treatment of refractive epilepsy, scientists from Australia in collaboration with IBM Research-Australia have used big data from epilepsy patients to develop a computer model that can predict when seizures will occur. So far, the technology predicts 69% of seizures in patients. While it’s still short of a range of accuracy making it feasible for use in patients outside of experimental settings, the acquisition of ever-increasing amounts of data will render the model more accurately.
The Art of Genetic Engineering
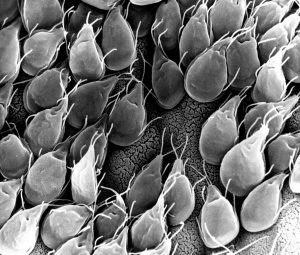
Among the techniques used in genetic engineering is protein folding, which is one of the naturally occurring processes that DNA undergoes as it takes on three dimensions. Among the major developments in genetic engineering was the discovery of the ability to fold DNA strands artificially, in a process called DNA origami.
Now, as suggested by the name “origami,” some people have begun using the process in quasi-artistic fashion. In an article recently published in Nature, bioengineers at CalTech led by Lulu Qian, Ph.D., assistant professor of bioengineering, showed they were able to produce a variety of shapes and designs using DNA origami, including a nanoscale replica of Leonardo da Vinci’s Mona Lisa.
DNA now also has another unique artistic application — tattoos, although people’s opinions of whether tattooing constitutes art might vary. Edith Mathiowitz, Ph.D., of Brown University’s Center for Biomedical Engineering, is among the patenters of Everence, a technology that takes DNA provided by a customer and incorporates it into tattoo ink. Potential tattooees can now have the DNA of loved ones incorporated into their bodies permanently, if they should so wish.
People and Places
The University of Washington has launched its new Institute for Nano-engineered Systems, cutting the ribbon on the building on December 4. The center will house facilities dedicated to scalable nanomanufacturing and integrated photonics, among others. Meanwhile, at the University of Chicago, Rama Ranganathan, M.D., Ph.D., a professor in the Department of Biochemistry and Molecular Biology and the Institute for Molecular Engineering, will lead that college’s new Center for Physics of Evolving Systems. Congratulations!
