Penn Engineers have developed a new means of targeting the lungs with lipid nanoparticles (LNPs), the miniscule capsules used by the Moderna and Pfizer-BioNTech COVID-19 vaccines to deliver mRNA, opening the door to novel treatments for pulmonary diseases like cystic fibrosis.
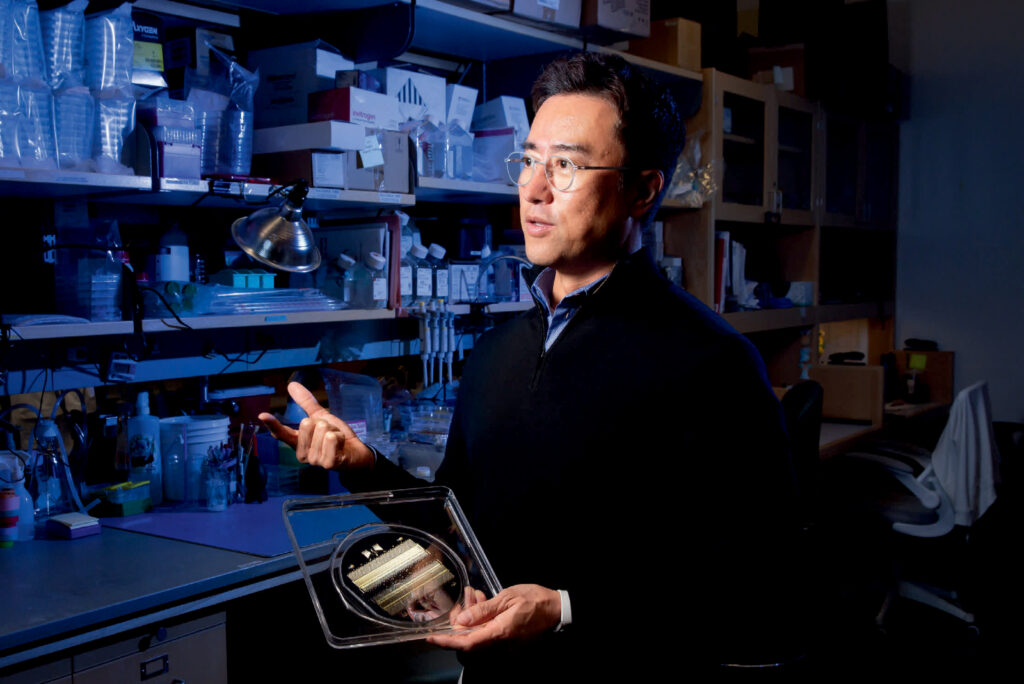
In a paper in Nature Communications, Michael J. Mitchell, Associate Professor in the Department of Bioengineering, demonstrates a new method for efficiently determining which LNPs are likely to bind to the lungs, rather than the liver. “The way the liver is designed,” says Mitchell, “LNPs tend to filter into hepatic cells, and struggle to arrive anywhere else. Being able to target the lungs is potentially life-changing for someone with lung cancer or cystic fibrosis.”
Previous studies have shown that cationic lipids — lipids that are positively charged — are more likely to successfully deliver their contents to lung tissue. “However, the commercial cationic lipids are usually highly positively charged and toxic,” says Lulu Xue, a postdoctoral fellow in the Mitchell Lab and the paper’s first author. Since cell membranes are negatively charged, lipids with too strong a positive charge can literally rip apart target cells.
Typically, it would require hundreds of mice to individually test the members of a “library” of LNPs — chemical variants with different structures and properties — to find one with a low charge that has a higher likelihood of delivering a medicinal payload to the lungs.
Instead, Xue, Mitchell and their collaborators used what is known as “barcoded DNA” (b-DNA) to tag each LNP with a unique strand of genetic material, so that they could inject a pool of LNPs into just a handful of animal models. Then, once the LNPs had propagated to different organs, the b-DNA could be scanned, like an item at the supermarket, to determine which LNPs wound up in the lungs.
Read the full story in Penn Engineering Today.