by Meagan Raeke

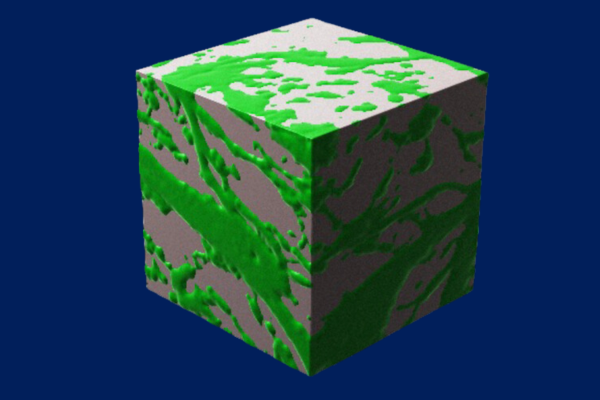
The effectiveness of CAR T cell therapy against a variety of cancers, including solid tumors, could be boosted greatly by using CRISPR-Cas9 technology to knock out the gene for CD5, a protein found on the surface of T cells, according to a preclinical study from investigators at the University of Pennsylvania’s Perelman School of Medicine and Abramson Cancer Center.
CAR T cells are T cells that have been engineered to attack specific targets found on cancer cells. They have had remarkable results in some patients with blood cancers. But they have not performed well against other cancers including solid-tumor cancers, such as pancreatic cancer, prostate cancer, and melanoma. Researchers have been searching for techniques to boost the effectiveness of CAR T cell therapy.
The study, published today in Science Immunology, suggests that knocking out CD5 could be a prime technique. Illuminating the protein’s previously murky role, the researchers found that it works as a powerful immune checkpoint, reining in T cell effectiveness. Removing it, they showed, dramatically enhanced CAR T cell anticancer activity in a variety of preclinical cancer models.
“We’ve discovered in preclinical models that CD5 deletion greatly enhances the function of CAR T cells against multiple cancers,” said senior author Marco Ruella, MD, an assistant professor of Hematology-Oncology, researcher with the Center for Cellular Immunotherapies and the scientific director of Penn Medicine’s Lymphoma Program. “The striking effects we observed across preclinical models suggest that CD5 knockout could be a general strategy for enhancing CAR T cell function.”
The study’s first author is Ruchi Patel, PhD, a recent graduate student from the Ruella Laboratory.
Read the full story in Penn Medicine News.
Marco Ruella is a member of the Penn Bioengineering Graduate Group. Read more stories featuring Ruella in the BE Blog.