In the human body, the lungs and their vasculature can be likened to a building with an intricate plumbing system. The lungs’ blood vessels are the pipes essential for transporting blood and nutrients for oxygen delivery and carbon dioxide removal. Much like how pipes can get rusty or clogged, disrupting normal water flow, damage from respiratory viruses, like SARS-CoV-2 or influenza, can interfere with this “plumbing system.”
In a recent study, researchers looked at the critical role of vascular endothelial cells in lung repair. Their work, published in Science Translational Medicine, was led by Andrew Vaughan of the University of Pennsylvania’s School of Veterinary Medicine and shows that, by using techniques that deliver vascular endothelial growth factor alpha (VEGFA) via lipid nanoparticles (LNPs), that they were able to greatly enhance modes of repair for these damaged blood vessels, much like how plumbers patch sections of broken pipes and add new ones.
“While our lab and others have previously shown that endothelial cells are among the unsung heroes in repairing the lungs after viral infections like the flu, this tells us more about the story and sheds light on the molecular mechanisms at play,” says Vaughan, assistant professor of biomedical sciences at Penn Vet. “Here we’ve identified and isolated pathways involved in repairing this tissue, delivered mRNA to endothelial cells, and consequently observed enhanced recovery of the damaged tissue. These findings hint at a more efficient way to promote lung recovery after diseases like COVID-19.”
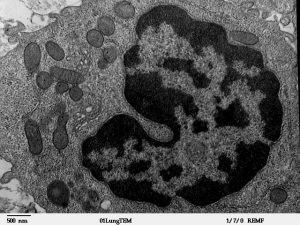
They found VEGFA’s involvement in this recovery, while building on work in which they used single cell RNA sequencing to identify transforming growth factor beta receptor 2 (TGFBR2) as a major signaling pathway. The researchers saw that when TGFBR2 was missing it stopped the activation of VEGFA. This lack of signal made the blood vessel cells less able to multiply and renew themselves, which is vital for the exchange of oxygen and carbon dioxide in the tiny air sacs of the lungs.
“We’d known there was a link between these two pathways, but this motivated us to see if delivering VEGFA mRNA into endothelial cells could improve lung recovery after disease-related injury,” says first author Gan Zhao, a postdoctoral researcher in the Vaughan Lab.
The Vaughan Lab then reached out to Michael Mitchell of the School of Engineering and Applied Science, whose lab specializes in LNPs, to see if delivery of this mRNA cargo would be feasible.
“LNPs have been great for vaccine delivery and have proven incredibly effective delivery vehicles for genetic information. But the challenge here was to get the LNPs into the bloodstream without them heading to the liver, which is where they tend to congregate as its porous structure lends favor to substances passing from the blood into hepatic cells for filtration,” says Mitchell, an associate professor of bioengineering at Penn Engineering and a coauthor of the paper. “So, we had to devise a way to specifically target the endothelial cells in the lungs.”
Lulu Xue, a postdoctoral researcher in the Mitchell Lab and a co-first author of the paper, explains that they engineered the LNP to have an affinity for lung endothelial cells, this is known as extra hepatic delivery, going beyond the liver.
Read the full story in Penn Today.