The growing threat of antimicrobial resistance demands innovative solutions in drug discovery. Scientists are turning to artificial intelligence (AI) and machine learning (ML) to accelerate the discovery and development of antimicrobial peptides (AMPs). These short strings of amino acids are promising for combating bacterial infections, yet transitioning them into clinical use has been challenging. Leveraging novel AI-driven models, researchers aim to overcome these obstacles, heralding a new era in antimicrobial therapy.
A new article in Nature Reviews Bioengineering illuminates the promises and challenges of using AI for antibiotic discovery. Cesar de la Fuente, Presidential Assistant Professor in Microbiology and Psychiatry in the Perelman School of Medicine, in Bioengineering and Chemical and Biomolecular Engineering in the School of Engineering and Applied Science, and Adjunct Assistant Professor in Chemistry in the School of Arts and Sciences, collaborated with James J. Collins, Termeer Professor of Medical Engineering and Science at MIT, to provide an introduction to this emerging field, outlining both its current limitations and its massive potential.
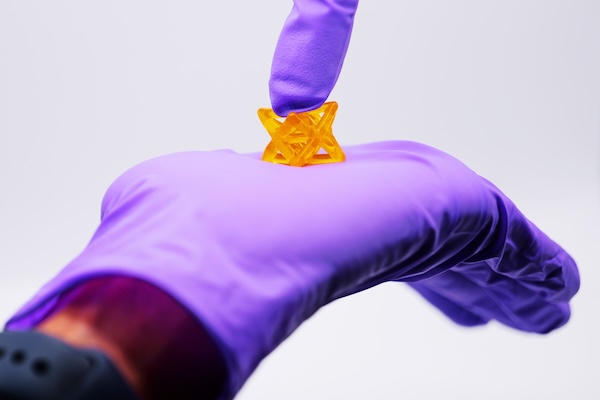
In the past five years, groundbreaking work in the de la Fuente Lab has dramatically accelerated the discovery of new antibiotics, reducing the timeline from years to mere hours. AI-driven approaches employed in his laboratory have already yielded numerous preclinical candidates, showcasing the transformative potential of AI in antimicrobial research and offering new potential solutions against currently untreatable infections.
Recent advancements in AI and ML are revolutionizing drug discovery by enabling the precise prediction of biomolecular properties and structures. By training ML models on high-quality datasets, researchers can accurately forecast the efficacy, toxicity and other crucial attributes of novel peptides. This predictive power expedites the screening process, identifying promising candidates for further evaluation in a fraction of the time required by conventional methods.
Traditional approaches to AMP development have encountered hurdles such as toxicity and poor stability. AI models help overcome these challenges by designing peptides with enhanced properties, improving stability, efficacy and safety profiles, and fast-tracking the peptides’ clinical application.
While AI-driven drug discovery has made significant strides, challenges remain. The availability of high-quality data is a critical bottleneck, necessitating collaborative efforts to curate comprehensive datasets to train ML models. Furthermore, ensuring the interpretability and transparency of AI-generated results is essential for fostering trust and wider adoption in clinical settings. However, the future is promising, with AI set to revolutionize antimicrobial therapy development and address drug resistance.
Integrating AI and ML into antimicrobial peptide development marks a paradigm shift in drug discovery. By harnessing these cutting-edge technologies, researchers can address longstanding challenges and accelerate the discovery of novel antimicrobial therapies. Continuous innovation in AI-driven approaches is likely to spearhead a new era of precision medicine, augmenting our arsenal against infectious diseases.
Read “Machine learning for antimicrobial peptide identification and design” in Nature Reviews Bioengineering.
The de la Fuente Lab uses use the power of machines to accelerate discoveries in biology and medicine. The lab’s current projects include using AI for antibiotic discovery, molecular de-extinction, reprogramming venom-derived peptides to discover new antibiotics, and developing low-cost diagnostics for bacterial and viral infections. Read more posts featuring de la Fuente’s work in the BE Blog.