Speaker: Susan N. Thomas, Ph.D.
Woodruff Associate Professor of Mechanical Engineering
Parker H. Petit Institute of Bioengineering and Bioscience
Georgia Institute of Technology
Date: Thursday, September 23, 2021
Time: 3:30-4:30 PM EDT
Zoom – check email for link or contact ksas@seas.upenn.edu
This virtual seminar will be held over Zoom. Students registered for BE 699 can gather to watch live in Moore 216, 200 S. 33rd Street.
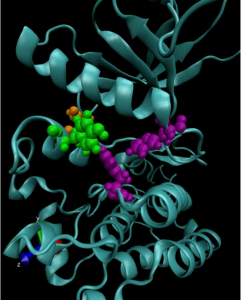
Abstract: Lymph nodes mediate the co-mingling of cells of the adaptive system to coordinate adaptive immune response. Drug delivery principles and technologies our group has developed to leverage the potential of lymph nodes as immunotherapeutic drug targets to augment anti-cancer therapeutic effects will be described.
Susan Thomas Bio: Susan Napier Thomas is a Woodruff Associate Professor with tenure of Mechanical Engineering in the Parker H. Petit Institute of Bioengineering and Bioscience at the Georgia Institute of Technology where she holds adjunct appointments in Biomedical Engineering and Biological Science and is a member of the Winship Cancer Institute of Emory University. Prior to this appointment, she was a Whitaker postdoctoral scholar at École Polytechnique Fédérale de Lausanne and received her B.S. in Chemical Engineering cum laude from the University of California Los Angeles and her Ph.D. as in Chemical & Biomolecular Engineering as an NSF Graduate Research Fellow from The Johns Hopkins University. For her contributions to the emerging field of immunoengineering, she has been honored with the 2018 Young Investigator Award from the Society for Biomaterials for “outstanding achievements in the field of biomaterials research” and the 2013 Rita Schaffer Young Investigator Award from the Biomedical Engineering Society “in recognition of high level of originality and ingenuity in a scientific work in biomedical engineering.” Her interdisciplinary research program is supported by multiple awards from the National Cancer Institute, the Department of Defense, the National Science Foundation, and the Susan G. Komen Foundation, amongst others.