by Evan Lerner

The COVID vaccines currently being deployed were developed with unprecedented speed, but the mRNA technology at work in some of them is an equally impressive success story. Because any desired mRNA sequence can be synthesized in massive quantities, one of the biggest hurdles in a variety of mRNA therapies is the ability to package those sequences into the lipid nanoparticles that deliver them into cells.
Now, thanks to manufacturing technology developed by bioengineers and medical researchers at the University of Pennsylvania, a hundred-fold increase in current microfluidic production rates may soon be possible.
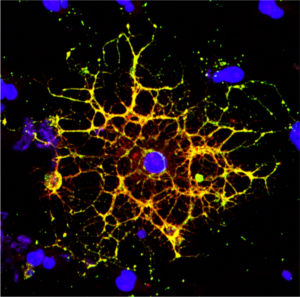
The researchers’ advance stems from their design of a proof-of-concept microfluidic device containing 128 mixing channels working in parallel. The channels mix a precise amount of lipid and mRNA, essentially crafting individual lipid nanoparticles on a miniaturized assembly line.
This increased speed may not be the only benefit; more precisely controlling the nanoparticles’ size could make treatments more effective. The researchers tested the lipid nanoparticles produced by their device in a mouse study, showing they could deliver therapeutic RNA sequences with four-to-five times greater activity than those made by conventional methods.
The study was led by Michael Mitchell, Skirkanich Assistant Professor of Innovation in Penn Engineering’s Department of Bioengineering, and David Issadore, Associate Professor in Penn Engineering’s Department of Bioengineering, along with Sarah Shepherd, a doctoral student in both of their labs. Rakan El-Mayta, a research engineer in Mitchell’s lab, and Sagar Yadavali, a postdoctoral researcher in Issadore’s lab, also contributed to the study.
They collaborated with several researchers at Penn’s Perelman School of Medicine: postdoctoral researcher Mohamad-Gabriel Alameh, Lili Wang, Research Associate Professor of Medicine, James M. Wilson, Rose H. Weiss Orphan Disease Center Director’s Professor in the Department of Medicine, Claude Warzecha, a senior research investigator in Wilson’s lab, and Drew Weissman, Professor of Medicine and one of the original developers of the technology behind mRNA vaccines.
It was published in the journal Nano Letters.
“We believe that this microfluidic technology has the potential to not only play a key role in the formulation of current COVID vaccines,” says Mitchell, “but also to potentially address the immense need ahead of us as mRNA technology expands into additional classes of therapeutics.”
Read the full story in Penn Engineering Today.






 NextUp, a regular feature of Philadelphia Magazine that “highlights the local leaders, organizations and research shaping the Greater Philadelphia region’s life sciences ecosystem,” ran a profile of Philly-based agricultural startup Strella Biotechnology. Founded by Penn alumna Katherine Sizov (Bio 2019) and winner of a 2019 President’s Innovation Prize, Strella Biotech seeks to reduce food waste through innovative biosensors, and was initially developed in the
NextUp, a regular feature of Philadelphia Magazine that “highlights the local leaders, organizations and research shaping the Greater Philadelphia region’s life sciences ecosystem,” ran a profile of Philly-based agricultural startup Strella Biotechnology. Founded by Penn alumna Katherine Sizov (Bio 2019) and winner of a 2019 President’s Innovation Prize, Strella Biotech seeks to reduce food waste through innovative biosensors, and was initially developed in the 